#96 How to Improve Metabolic Health with HIIT, Circadian-Timed Eating, & Sleep
This episode is available in a convenient podcast format.
These episodes make great companion listening for a long drive.
The Omega-3 Supplementation Guide
A blueprint for choosing the right fish oil supplement — filled with specific recommendations, guidelines for interpreting testing data, and dosage protocols.
Exercise, meal timing, and sleep. What do they have in common? They’re the foundation of a healthy lifestyle. I also consider them to be straightforward areas to tackle when it comes to longevity strategies. They do require effort to implement, but doing so is incredibly simple.
The good news is that because there are several levers to pull, we don't have to choose just one. But we do need to be diligent about taking action to support our longevity. This begins with optimizing our metabolic health.
Metabolic health has ramifications that extend far and wide. Our body’s ability to regulate blood glucose levels stands out as one of the most important metrics predicting long-term health.
Even having high plasma glucose levels that fall within the normal range is associated with greater atrophy of the hippocampus and amygdala—two structures in the brain with relevance to aging and neurodegenerative processes. Having a high HbA1c, which is considered a long-term marker of glucose regulation, leads to the formation of advanced glycation end products or AGEs. AGEs can crosslink with protein and lipids, including collagen, reduce the elasticity of our heart and contribute to a stiffening of blood vessels, and promote high blood pressure, putting us at risk for cardiovascular disease.
It’s clear that we should be doing all that we can to improve our metabolic function throughout life.
Recently, I gave a talk at the American Academy of Anti-Aging Medicine (A4M) conference in Palm Beach, Florida where I presented my top three strategies for optimizing metabolic health:
- High-intensity interval training (HIIT)
- Circadian-timed eating
- Quality sleep
Some highlights from this episode:
-
Why HIIT outshines moderate-intensity exercise for improving metabolic health
-
How lactate accumulation from higher training intensity benefits glucose homeostasis
-
The optimal HIIT conditions for improving body composition
-
How vigorous exercise boosts mitochondrial repair through mitophagy
-
Evidence-based HIIT protocols (Tabata, Wingate, 1-minute on/1-minute off, and Norwegian 4x4)
-
Just 10 reps of this exercise every 45 minutes is more powerful at improving glucose homeostasis than a 30-minute walk
-
How to improve postprandial glucose regulation with "exercise snacks"
-
Why it's beneficial to time meals with melatonin release
-
Can high-normal glucose levels shrink your hippocampus?
-
How even mild sleep restriction creates a metabolic profile similar to type 2 diabetes
-
Why just 1 hour of extra sleep might help you lose weight
-
How to ameliorate the increased mortality risk associated with sleeping less than 7 hours a night
High-intensity interval training (HIIT)
“HIIT provides an opportunity for people to have a time-efficient way for improving their metabolic health.” - Dr. Rhonda Patrick Click To Tweet
HIIT is a time-efficient training technique that involves short, intense bursts of physical activity alternated with brief recovery periods or light exercise. The metabolic benefits of HIIT include:
- Improved triglycerides and glucose regulation
- Increased insulin sensitivity
- Decreased fat mass and improved body composition
- Enhanced mitochondrial function
HIIT outperforms moderate-intensity continuous exercise, leading to greater improvements in:
- Cardiorespiratory fitness (e.g., VO2 max)
- Systolic and diastolic blood pressure
- High-density lipoproteins
- Triglycerides
- Fasting blood glucose
- Oxidative stress and inflammation
- Appetite-regulating hormones and beta-cell function
- Markers of mitochondrial biogenesis
- Cardiac function
What explains the unique benefits of HIIT?
During high-intensity exercise, our mitochondria and muscles undergo a significant energetic stress—our body can’t keep up with energy production via fat metabolism alone, so our body switches to using glucose and glycogen (glycolysis) for ATP production. In the process of breaking down glucose, lactate is produced. Rather than a toxic byproduct, lactate can be used as a source of energy for the body and the brain.
But that’s not all, lactate is also a potent signaling molecule that allows for cross-talk between our muscles and other organs throughout the body. Among its other signaling effects, lactate increases GLUT4 transporters in skeletal muscle, allowing for a greater amount of glucose uptake. This effect lasts for up to 48 hours, with the first 24 hours representing the most robust period of enhanced glucose control.
The optimal HIIT protocol to improve body composition
High-intensity training reduces fat mass and body fat percentage and increases fat-free mass (i.e., lean body mass). Running and cycling HIIT protocols appear to be the most effective, especially when the following parameters are adhered to:
- Duration: More than 8 weeks of training
- Frequency: At least 3 sessions per week
- Interval structure: Less than 60 seconds per interval with 90 seconds or less of active recovery
HIIT corrects mitochondrial dysfunction in type 2 diabetes
“Lactate is consumed by other organs…and it’s serving as a very utilizable source of energy. But one of its most important roles is as a signaling molecule.” - Dr. Rhonda Patrick Click To Tweet
People with type 2 diabetes demonstrate markers of mitochondrial dysfunction, characterized by 40% lower mitochondrial respiration and enlarged, fragmented mitochondria, indicative of mitochondrial damage. These structural and functional changes are correlated with insulin resistance.
High-intensity exercise increases a cellular repair process known as mitophagy—it sends a signal to clear out and recycle damaged or dysfunctional mitochondria. In this way, long-term exercise training leads to more and healthier mitochondria. Mitophagy is a similar process to autophagy, which is enhanced during intermittent fasting or periods of low energy availability. But exercise appears to be a much more robust signal for mitophagy than fasting. In fact, exercise enhances mitophagy whether or not it’s performed in the fasted state.
HIIT also enhances mitochondrial biogenesis in skeletal muscle in addition to increasing the effectiveness and efficiency of existing mitochondria. This is the result of the potent effects of lactate, which send a signal to the body to increase mitochondria as an adaptation to produce more energy.
Other metabolic benefits of HIIT occur through increasing a muscle protein called PGC-1α. Higher levels of PGC-1α can improve muscle's oxygen use, antioxidant defense, and glucose management, and may also protect against muscle loss with aging and reduce inflammation.
HIIT protocols to improve metabolic health
- Tabata training: Tabata training involves performing 8 intervals total alternating between 20 seconds at 170%+ of VO2 max and 10 seconds of rest. Not including the warmup and cooldown, this workout takes 4 minutes to complete.
- Wingate intervals: Wingate training, named for the exercise test for which this workout was named, involves performing 4–6 intervals total. The hard portion is 30 seconds at an “all out” intensity followed by 4 minutes of rest or active recovery. Not including a warmup and cooldown, this workout takes 18–27 minutes to complete.
- 1-minute on/1-minute off training: This protocol involves performing 10 intervals total alternating between 60 seconds at 90%+ of heart rate reserve and 60 seconds of rest or active recovery. Not including a warmup and cooldown, this workout takes 20 minutes to complete.
- Norwegian 4x4 training: Named because it’s performed by the Norwegian ski teams, this workout involves performing a total of 4 intervals alternating between 4 minutes at 85–95% of maximal heart rate and 3 minutes at 60–70% of maximal heart rate. Not including a warmup and cooldown, this workout takes 25 minutes to complete.
Exercise snacks to improve metabolic health
Exercise snacks are brief bouts of high-intensity exercise (75% or more of maximum heart rate) performed intermittently throughout the day for 1–2 minutes.
Examples of exercise snacks include:
- High knees
- Lunges
- Stair sprinting
- Jump squats
- Chair squats
Strategically timing exercise snacks 30–60 minutes before or after meals appears to markedly improve glucose regulation, regardless of whether or not someone has insulin resistance.
Exercise snacks also improve longevity: People who engage in ~3 bouts of exercise snacks/vigorous intermittent lifestyle physical activity (VILPA) per day (each lasting 1–2 minutes) have a 40–50% reduction in all-cause, cancer, and cardiovascular disease mortality compared to people who don’t engage in exercise snacks.
Circadian-timed eating
“People that do early time-restricted eating without reducing their calorie intake dramatically improve a variety of metabolic parameters.” - Dr. Rhonda Patrick Click To Tweet
-
High-Intensity Interval Training (HIIT)
-
How HIIT has been shown to be more effective than moderate exercise in improving insulin resistance, HbA1C levels, body weight, and fasting glucose
-
How a systematic review showed that HIIT outperforms moderate exercise in improving CRF, lowering BP, and enhancing metabolic and cardiac function
-
How mitochondria struggle to meet energy demands during high-intensity exercise, causing muscle cells to shift to glycolysis for glucose use, which results in lactate production
-
How Dr. George Brooks discovered that lactate, once thought to be a metabolic byproduct, is actually an important signaling molecule consumed by organs like the brain and heart, and how it boosts glucose uptake in muscles
-
How steady-state lactate levels differ from levels achieved during exercise
-
How lactate, beyond its role as an energy substrate, acts as a key signaling molecule, increasing GLUT-4 transporters in muscles and improving glucose homeostasis long after exercise
-
Optimal HIIT conditions for improving body composition (including training duration, frequency, and specific interval and recovery timings)
-
How mitochondria differ in people with metabolic syndrome, type 2 diabetes and obesity
-
How vigorous exercise boosts mitochondrial repair through mitophagy
-
How HIIT enhances mitochondrial biogenesis, increasing mitochondrial volume, while also promoting mitophagy, offering a double benefit of repair and new mitochondrial growth.
-
How lactate generated during HIIT activates PGC1-alpha, stimulating mitochondrial biogenesis in muscle, which improves energy efficiency, reduces atrophy, and enhances exercise endurance
-
How the body's adaptation to vigorous exercise, by producing more mitochondria, is especially beneficial for those with type 2 diabetes and obesity
-
Evidence-based HIIT protocols
-
Exercise Snacks & Vigorous Intermittent Lifestyle Physical Activity (VILPA)
-
How evidence suggests that interrupting prolonged sitting with short, frequent walking or squatting breaks is more effective at improving postprandial glycemic control in overweight and obese men than a single 30-minute walk.
-
Why timing exercise snacks 30 minutes to 1 hour before or after meals improves postprandial glucose regulation
-
How as little as three to four minutes of Vigorous Intermittent Lifestyle Physical Activity (VILPA) activity per day significantly reduces the risk of cardiovascular, cancer, and all-cause mortality
-
How to incorporate exercise snacks in your workday
-
Circadian-Timed Eatin
-
Why morning insulin sensitivity is higher, driven by circadian rhythms and melatonin's effect on beta cells, and how genetic variation in the melatonin receptor 1B increases the risk of type 2 diabetes
-
Why it's beneficial to time meals with melatonin release, including the recommendation to finish your last meal 3 hours before bedtime and wait an hour after waking for breakfast to allow melatonin to clear
-
How bright light exposure in the morning hastens the clearance of melatonin and why this affects the optimal timing for meals
-
Evidence from a UK Biobank study suggests that even high-normal glucose levels, below diabetic or prediabetic ranges, are linked to hippocampal shrinkage
-
Evidence suggests that circadian misalignment from jetlag, shift work, and erratic sleep leads to glucose dysregulation, raising glucose and insulin levels, with postprandial glucose reaching prediabetic levels. It also lowers leptin, increasing appetite.
-
Time-restricted eating (TRE) in shift workers, based on Satchin Panda's studies in firefighters, improves metabolic health, glucose regulation, insulin sensitivity, and reduces blood pressure, even without calorie reduction
-
Whether time-restricted eating requires a reduction in calorie intake and how it can improve metabolic health, even without cutting calories
-
Whether a 10-hour eating window is sufficient to deliver the significant health benefits associated with time-restricted eating
-
Early time-restricted eating (TRE) is more effective than late TRE, as shown by a meta-analysis of 12 RCTs, with better improvements in insulin resistance, blood pressure, and weight loss
-
Sleep
-
How poor sleep disrupts glucose homeostasis, with even mild sleep restriction (1-3 fewer hours for 3 nights) leading to increased fasting insulin, higher insulin during OGTT, elevated glucagon, and decreased insulin sensitivity
-
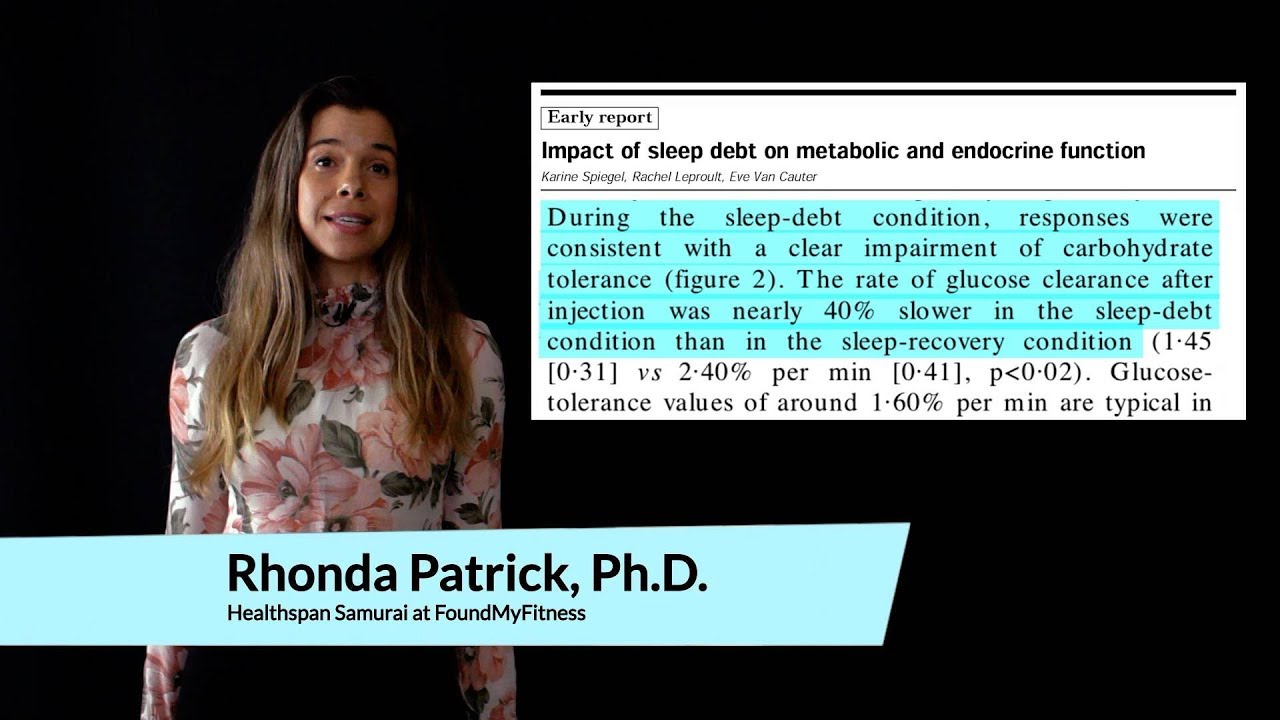
How sleep debt, such as 3 days of only 4 hours of sleep per night, slows glucose clearance by 40%, decreases glucose effectiveness by 30%, and reduces insulin response by 30%, mimicking early signs of diabetes
-
The optimal sleep duration for minimizing type 2 diabetes risk
-
How chronically elevated blood sugar levels lead to the formation of advanced glycation end products (AGEs), which stiffen collagen, cause hypertension, reduce arterial flexibility, increase cardiovascular disease risk, and worsen with age
-
What 4 hours of sleep for 4 nights does to insulin signaling in adipocytes
-
How sleep loss promotes an obesogenic appetite profile, with just 2 days of 4 hours less sleep decreasing leptin, increasing ghrelin, and making people hungrier, particularly craving carbs, salty, and processed foods
-
The importance of bright morning light exposure, avoiding blue light at night, and creating a dark room environment for better sleep quality
-
How melatonin regulates body temperature, and how optimizing room temperature can improve sleep quality
-
The importance of finishing meals 3 hours before bedtime to support melatonin production and improve sleep quality
-
How regular exercise acts as a zeitgeber, supporting the body's internal clock to improve circadian rhythm, enhance daytime alertness, and promote better sleep
-
Why monitoring caffeine intake is important for sleep, as each cup can shift circadian rhythms by 45 minutes, with individual variation in sensitivity
-
Why 1 hour of extra sleep could help you lose weight
-
How Cognitive Behavioral Therapy for Insomnia (CBTI) improves sleep
-
Combating Sleep Restriction With HIIT
-
How HIIT counteracts sleep-induced acute insulin resistance, with studies showing that 3 sessions over 5 days can improve circadian rhythm, glucose tolerance, and mitochondrial function, even during sleep restriction
-
Why HIIT combats sleep-restriction-induced glucose dysregulation
-
How preemptive HIIT sessions enhance glycemic control, helping to prevent high blood sugar and insulin resistance caused by sleep loss or jet lag
-
Can HIIT ameliorate the mortality risk from poor sleep?
So glad to be here. I want to thank the organizers at a four m for inviting me to speak. I spoke at Longevity fest last December. It was amazing. So I'm super pumped to be here today talking all about metabolic health. And we're really going to. We're going to focus on what I think are three major lifestyle factors that can play a pretty big role in the metabolic health. So we're going to be talking about. Sorry, is this not working? All right, we'll be talking about high intensity interval training, which is a very time efficient way to get your heart rate up to improve insulin sensitivity, glucose homeostasis, glucose transport, mitochondrial function. And we're going to talk a little bit about exercise snacks that can be strategically timed and how that can play a profound role in glucose homeostasis. We're going to talk about circadian timed eating. So why it's important to avoid late night eating, what the effects of melatonin are on insulin, time restricted eating and circadian misalignment. And then we're going to jump into sleep and the profound metabolic effects of sleep restriction on metabolic health, as well as some behavioral changes that can be implemented to improve metabolic health. So let's start with high intensity interval training. So, as I mentioned, this is a very time efficient way to get your heart rate up and exercise. So it involves very short bouts of intense exercise. One, we're talking about heart rate up at least 75% max heart rate followed by periods of recovery. There's a lot of different protocols we're going to discuss, but there have been lots of studies talking and showing that high intensity renal training can improve glucose homeostasis, insulin sensitivity. It also decreases fat mass, improves body composition and enhances mitochondrial function. So a meta analysis of 50 different randomized controlled trials compared high intensity interval training to moderate intensity continuous exercise. So this would be exercise that's at a lower intensity, the kind of intensity where you can have a conversation but you're maybe still breathy, sometimes called zone two. And this is a longer duration type of exercise. So, high intensity interval training outperforms moderate intensity continuous exercise at decreasing insulin resistance. It also improves HBA one c levels. So the long term biomarker for elevated blood glucose levels, it leads to a decrease in body weight and also significantly lowers fasting blood glucose levels. Again, this is 50 different randomized controlled trials. And another systematic review of many different randomized controlled trials has found that, again, high intensity interval training outperforms moderate intensity continuous exercise at improving cardiorespiratory fitness, improving diastolic and systolic blood pressure, improving hdl triglycerides and fasting glucose, lowering oxidative stress, improving adiponectin and insulin sensitivity, as well as beta cell function to produce insulin. It increases PGC one alpha, which is a biomarker for mitochondrial biogenesis, which we'll be discussing in a little bit. And it also improves cardiac function. And this is all better than moderate intensity continuous exercise. So it really provides an opportunity for people to have a time efficient way of improving metabolic health. And part of that is because when you get your heart rate up high, when you are putting in the effort, you're putting a strong stress on your mitochondria, and your muscle. And your mitochondria are unable to produce energy quick enough to keep up with the demand. And so your muscle cells shift to using glucose as a source of energy through glycolysis. And that ends up producing lactate, which was thought to be a byproduct, a metabolic byproduct. Well, a couple of decades ago, Doctor George Brooks at the University of California in Berkeley was one of the pioneers to find that lactate generated from exercise is anything but a byproduct. So steady state lactate levels are less than one millimolar. When you crank up the intensity of exercise, you can go anywhere up to 1517 millimolar. And that lactate, it gets in circulation and it's consumed by other organs. It goes into the brain, it goes into the heart, it goes back into the muscle, it goes to the kidneys, it goes to the liver, and it's serving a very utilizable source of energy. So lactate can be used and converted into acetyl CoA and used by energy by the mitochondria. But probably one of its most important roles is as a signaling molecule. It's a way for your muscle to connect, to communicate with other organs and other tissues. And one of its signaling roles is back in the muscle. It's increasing the translocation of glucose, four transporters to the cell surface of the muscle. Glut, four transporters. And so lactate gets back into the muscle. It's basically telling the muscle, hey, we're using a lot of glucose here for energy, so we need to bring more glucose in. And the way it does it is by increasing glut. Four transporters at the muscle. And I mentioned lactate levels go up during this intense exercise. That's very transient. So after about 20 minutes, when exercise stops, your lactate levels go back to baseline, because all these other organs, including the muscle, are consuming it so quickly. However, the increase in glucose for transporters stays elevated for up to 48 hours, with the first 24 hours being the most robust. So you're getting a long term effect from that signaling from lactate back to the muscle to increase glut four transporters. And that is why high intensity interval training is so potent and powerful at improving glucose homeostasis. So there was another meta analysis of 36 randomized controlled trials that were looking at optimal conditions of high intensity level training for improving body composition. And so it's been identified that the duration of the hit workout, high intensity nipple training workout, eight weeks, is optimal for improving body composition. The frequency is at least three sessions a week, and the intervals are 60 seconds or less of the robust, intense interval, followed by about 90 seconds of recovery. And this leads to improvements in reducing fat mass. Cycling and running was the best at doing that, also improving percent body fat. So body fat reduction, and that was the best with running and then increasing fat free mass, which includes muscle, and the best at that was actually cycling. So these are some of the optimal conditions for improving body composition. With respect to high intensity interval training protocols. We're going to talk about how high intensity interval training can regulate mitochondrial function. But before we talk about that, I think it's important to recognize that people with metabolic syndrome, insulin resistance, obesity and type two diabetes have been identified to have pretty profound dysregulated mitochondria. So the mitochondria and skeletal muscle from people with type two diabetes and obesity have been found in multiple studies to respire about 40% less than skeletal muscle cells from people that do not have type two diabetes or people that are lean. So their mitochondria are dysfunctional. And subsequent studies have also identified structural defects in the mitochondria. So mitochondria from people with type two diabetes are fragmented. So mitochondria are typically, they form a very connected network. This sort of look like vermicelli spaghetti. And that's a really beautiful network of mitochondria that are able to undergo respiration and do their functions quite robustly. When mitochondria become really fragmented, they are dysfunctional, they can't utilize or even produce energy very well, and they're on their way to basically dying and causing cells to die. So there's a very intricate connection between structure of mitochondria and the function of mitochondria. And that's important because vigorous exercise, high intensity exercise, has been shown to increase this repair process in mitochondria, known as mitophagy so when exercise is intense enough, it increases the nutrient sensing protein amp kinase ampk, it activates it. And this causes the mitochondria to send the signal that they need to repair themselves. And so mitochondria can be sort of dysfunctional or they can be really dysfunctional. So mitophagy can clear away an entire dysfunctional mitochondria to be used and recycled, or it can clear away pieces of a dysfunctional mitochondria. So when you're doing that acute exercise, your mitochondria, if you have a dysfunctional one, the mitophagy pathway gets activated and the mitochondria fizzes off. It kind of goes through this mitochondrial fission process, and that damaged part of the mitochondria then goes and is recycled through the lysosome. And then what you have is a long term effect of, after doing routine, high intensity exercise, you then have more healthy functional mitochondria because you're just getting rid of the damaged part of the mitochondria. If the mitochondria is dysfunctional enough, you're going to get rid of the whole mitochondria. And by the way, the Amp kinase pathway, many of you are probably thinking, oh, well, that's a nutrient sensing pathway. It's activated during periods of, of fasting. And that is true. AmP kinase is activated during periods of fasting. And fasting is a powerful signal for inducing autophagy and mitophagy. However, in this particular study, people that did this high intensity, vigorous exercise for 30 minutes, it did not matter if they had fasted for 16 hours or not. There was no difference in the mitophagy. So, in other words, the exercise itself was such a strong signal for activating mitophagy that it didn't matter if they had not fasted for 16 hours because it was so powerful on top of the repair process. High intensity interval training is one of the most robust exercise modalities that can increase mitochondrial biogenesis. So the growth of new mitochondria, increasing mitochondrial volume. So you're having this double whammy effect where you're getting repairing of the mitochondria, getting rid of the unhealthy parts, and then you're increasing the growth of new mitochondria. So one of the reasons high intensity interval training is very good at increasing mitochondrial biogenesis compared to, let's say, moderate continuous exercise, is because lactate that's generated from that vigorous exercise is a signaling molecule to activate the protein that very much regulates mitochondrial biogenesis. And skeletal muscle, PGC one alpha. So, again, lactate is playing that signaling role. It's generated by the muscle, it's taken back up by the muscle, and then it's communicating with the muscle. It's saying, hey, we can't make energy fast enough because this exercise is so intense, we need more mitochondria to be able to do that. So it's an adaptation to the vigorous intensity exercise. And that adaptation is making more mitochondria, which is obviously very beneficial for not only people with type two diabetes, metabolic syndrome, obesity, but also everybody. So mitochondrial biogenesis improves energy efficiency in mitochondria and also is associated with other benefits, like decreased atrophy and improved exercise endurance as well. So there's a whole host of benefits with increasing mitochondrial biogenesis. So a lot of the high intensity interval training protocols that were used in these systematic analysis and these meta analyses were evidence based HIIT protocols. So tabata is one that's used. That's a 22nd on, ten second off interval, 20 seconds. At the highest intensity you can do, you're going all out, and then you're resting for 10 seconds, and that's repeated eight times for a total of a four minute workout. In some cases, the Tabata protocol was repeated twice. The wing gait HIIT protocol is another very commonly used one. And that is a 32nd all out sprint followed by four minutes of active recovery, where you're low intensity. And then you do that four to six times. That's about a 20 minutes or so workout. And then there's the conventional workout. It's the 1 minute on, 1 minute off. So you're going as intense as you can for 1 minute, and then you have 1 minute of very light active recovery, and then you repeat that ten times. That's a 20 minutes workout. It is hard, but it's very, very effective at improving a variety of metabolic parameters. And then there's the clinical workout, also known as the Norwegian four X four, which I like to call it because the norwegian ski team often uses this HIIT protocol for their training. It's a four minute interval where you're going as intense as you can for four minutes, and then you have light recovery for three minutes. So you're going very, very light getting your heart rate down. And that's repeated four times. So it's about a 25 minutes workout. So let's just talk a little bit about exercise snacks, which is a type of high intensity interval training workout. It involves doing something at vigorous intensity, you know, a vigorous intensity heart rate for one to two minutes. And they're often called exercise snacks because you can just do them whenever, throughout the day. And I think this is very relevant because I just came across a study a couple of weeks ago that showed ten body weight squats. Okay? Ten for every 45 minutes was more powerful at improving glucose homeostasis than a 30 minutes walk. So I feel like that is. It kind of puts it in context, because how easy is it to get up and do ten body weight squats, right, every 45 minutes? I mean, it doesn't get easier than that. And there's also a reason to strategically time these exercise snacks either 30 minutes to an hour before a meal or 30 minutes to an hour after a meal. So the timing of these exercise snacks has been shown in several studies. People with type two diabetes or insulin resistance, to really improve their glucose regulation after a meal. So their postprandial glucose regulation and their glucose disposal was improved again, because getting that high intensity exercise where you're generating some lactate, it's increasing glute, four transporters of the muscle, and that is then causing glucose to come into the muscle. It's lowering the burden of your pancreas to have to produce insulin, and it's improving glucose homeostasis. So exercise snacks around meals is an easy way to improve postprandial glucose regulation and glucose homeostasis. It's obviously very relevant for people with type two diabetes, but also, I think, for everyone. Exercise snacks has also been associated with a decrease in all cause mortality. So there have been very large studies out of the UK biobank data where people are wearing accelerometers and they're part of the vigorous intensity. Sorry, vigorous, intermittent lifestyle activity studies that have been done. Vilpa, they're called, and what those studies have identified is that people that do one to two minutes of vigorous intensity exercise, and these are things like just sprinting up the stairs rather than taking the escalator or walking up the stairs, and they do this, this like a one to two minute, high intensity burst, and they do this three times a day. That's associated with a 50% reduction in cardiovascular related mortality. 50% reduction. It's also associated with a 40% reduction in cancer related mortality and all cause mortality. So, cancer, cardiovascular disease, these are all diseases that are associated with metabolic dysregulation. So implementing exercise snacks, I think, is one of the easiest ways to get, you know, get a little bit of exercise, get your heart rate up, get that lactate generated, increase your glucose transporters, but also just improve your mood to break up your sedentary time, you know? So being sitting at your desk for a couple of hours is sedentary. And being sedentary is an independent risk factor for certain diseases like cancer. So, I mean, we've all been sitting here for what, an hour at least. I say we get up and we do a minute of bodyweight squats. Bodyweight squats. All right, ready? Okay, I'm going to get this timer going. We're going to do a whole minute. I'm saving you the high knees. All right, here we go. So we're going to do bodyweight squats. We're going to try to get the heart rate up and we're going to do it for 1 minute. Try to go low if you can. You want to feel the burn in your quads. I'll go sideways there. Keep going. We're not even at 30 seconds yet. Okay, we're halfway. Are you guys getting your heart rate up? Are you feeling it? 15 seconds left. 5432. All right, so a little out of breath, feeling good. Increase the blood flow to the brain, but more importantly, glute four transporters. Okay, so we're going to shift gears and we're going to talk a little bit about circadian meal timing. All right? Okay, so as everybody here knows about circadian rhythm, we're all diurnal creatures here, more active during the day, less active in the evening. Right. Our metabolism is also on a circadian rhythm. We are more insulin sensitive earlier in the day and later in the evening, less insulin sensitive, part of that. So let me talk about a study that I think is pretty telling in terms of insulin sensitivity and glucose regulation throughout the day. So participants were given the same exact meals in the morning, in the afternoon, or in the evening. Okay, so same macronutrient composition, same caloric content, everything the same. And participants were much more insulin sensitive in their first meal, given in the morning compared to their evening meal. And I think part of this has to do with our circadian rhythm and as we get later in the day, melatonin. So back in, like the early two thousands, about 2009, a lot of studies started coming out in the genetics world, where a certain variation in the melatonin receptor one b was identified to be a pretty high risk factor for developing type two diabetes and for having basically insulin dysregulation. So people were not producing insulin correctly. And it was very perplexing to scientists at the time because melatonin was thought to be just this hormone that is produced by the pineal gland that is regulating our sleep, it's quieting down our brain, telling us it's time to get sleepy. Right? It's making us tired. Well, it turns out, after more studies started to investigate this, that we have melatonin receptors on our pancreas, on our pancreatic beta eyelid cells. And the melatonin receptors, the one b receptors, are sensitive to melatonin. People with that gene variation had a hypersensitive receptor wherever little bits of melatonin were enough to really kind of activate it. And so it turns out melatonin is also quieting down our pancreas at night and telling our pancreas we don't have to produce so much insulin. It's nighttime, we're not going to be eating. And so there's a systemic effect of melatonin not only on our brain, but also on our other organs that are important for metabolism. And I think this is a really good reason to think about when you're going to have your last meal and why it is detrimental to engage in late night eating. So our bodies naturally produce melatonin about three or so hours before our natural bedtime. So it's a good rule of thumb to make sure that you have finished your last meal, you finished eating before that time. So before 3 hours before your natural bedtime, it's really just a good rule of thumb to kind of make sure you're done eating. Then when you wake up in the morning, you're also still producing some melatonin for about the first hour. Now, bright light exposure can inhibit that, so it can hasten the clearance of the melatonin. But also I think it's a good idea to wait about an hour after you first wake up before you start taking in your meal. So bright light exposure, we'll talk about. Also it's very important for regulating our circadian rhythm and that's important for sleep. But generally speaking, I think just aligning your meals with your circadian rhythm, it makes sense when you think about the role of melatonin, you know, in quieting down our brain and also our pancreas. It makes a lot of sense why you don't want to be eating late at night. So just as a, you know, I think an aside here, having glucose levels in the normal range, but on the high normal range, so high normal glucose was associated in uk biobank data with higher incidence of atrophy in the hippocampus. So the part of the brain involved in learning and memory. So people that just had higher than they were on the high end of normal had more atrophy in their hippocampus than people on the low end of normal. So this is in the absence of any clinical type two diabetes, really sort of highlighting the importance of everyone considering their metabolic health. Even if you don't have type two diabetes, even if you're nothing, you know, pre diabetic, you just, you want to make sure that your. Your glucose regulation is, you know, the best it can be. Circadian misalignment. Now, so many of you may have come from, like me, the west coast, or perhaps Europe, and you're out of sync with your circadian rhythm. So circadian misalignment refers to when your natural internal clock is out of sync based on a behavioral pattern. So this is very common with jet lag. It's very common in shift workers who are up in the night, in the evening, working and eating. It's also very common in people with erratic sleep behaviors. So there's been studies done where people, participants are, they're circadian misaligned, so they're the out of sync. So basically their sleep and meals are shifted by about 12 hours. And when that happens, people have about a 6% increase in their glucose. They make 22% more insulin. They have decreased leptin levels, so that's the hormone involved in being satiated. And their postprandial glucose levels are in the pre diabetic range only by shifting their circadian clock by 12 hours. So it has a profound effect. Being circadian misaligned exercise can help with that, especially high intensity interval training, but also time restricted eating. So time restricted eating refers to eating all your food in a restricted window of time instead of just eating ad libitum right throughout the day. And typically time restricted eating is anywhere between six to 10 hours of an eating window, and the rest is fasting. There's been a lot of work done by Doctor Sachin Panda on time restricted eating in shift workers. He's done some work on firefighters showing these firefighters that are up all night, if they eat their food in a time restricted eating window, you know, 8 hours, 10 hours, that it improves their metabolic biomarkers. So there's been a lot of meta analyses done on time restricted eating and how it improves metabolic health. Now, time restricted eating does not mean you have to reduce your calorie intake. But we're going to talk about in a minute, people that are naturally doing time restricted eating tend to do that because they're skipping snacks or they're skipping their dessert or they're skipping a meal. So when people do end up reducing their calorie intake along with time restricted eating. They end up losing weight and losing fat, but independent of calories. So if they do not change their caloric intake but they are practicing time restricted eating, it can improve glucose regulation, insulin sensitivity, it can lower blood pressure. And so there's a lot of metabolic parameters that are improved with just the time restricted eating. Now, as I mentioned, people that do practice time restricted eating, so there's been multiple studies looking at even just a ten hour window, which isn't even that restricted. People that are doing a ten hour time restricted eating window, not a controlled trial, but just like you tell them to do it, they end up reducing, on average, about 200 calories a day, again, because typically people are skipping snacks or meals. And so that does lead to weight loss, and it reduces waist size, body fat percentage and also reduces visceral fat, which is the deep fat that surrounds your organs, that's secreting pro inflammatory cytokines and hormones that play a role in type two diabetes metabolic syndrome. But also emerging evidence indicates visceral fat plays a role in cancer as well. Time restricted eating also lowers blood pressure. It improves lipid profiles and improves the HBA. One circumental glucose biomarker, early time restricted eating. So this is typically people that end their last meal at about 04:00 p.m. usually, early time restricted eating is about a six hour window, so it's a shorter eating window. People that do early time restricted eating without reducing their calorie intake dramatically improve a variety of metabolic parameters. Insulin levels are improved. Insulin sensitivity is improved. Beta cells are more responsive to glucose. The improvements in blood pressure were so profound that they were equivalent to some antihypertensive treatments. So that was a big finding of that study. And then oxidative stress levels were also improved. And this is early time restricted eating. There's been a meta analysis of about twelve randomized controlled trials looking at early time restricted eating. Again, this was defined at stopping your last meal at about 04:00 p.m. and then comparing it to later time restricted eating. So people that were stopping their meals not at four, but a little bit later, and all the eating windows were either six, sorry, four to 10 hours. And early time restricted eating does have more profound effects on glucose regulation, largely because, again, we're more insulin sensitive earlier, less insulin sensitive later. Once the melatonin starts to kick in again, that just, it gets much worse. So early time restricted eating can improve fasting blood glucose levels and insulin resistance more than late later time restricted eating, but it also has a more profound effect on the blood pressure regulation, so lowering blood pressure. Late time restricted eating can sort of maintain blood pressure, but it doesn't improve it like the early time restricted eating. And both early and late improve lipid profiles as well as fasting glucose and insulin resistance. Just early does it a little bit more robustly. So I think there's pretty strong evidence that if you are circadian misaligned jet lag, for example, if you're a shift worker, or just people that are wanting to sort of try to optimize their glucose homeostasis as much as possible. Certainly people with metabolic dysfunction may benefit from time restricted eating, along with the high intensity training and the ten body weight squats every 45 minutes. Okay, so let's talk about the last topic I want to discuss this morning, and it has to do with poor sleep and how most of us, I think, are aware when we don't get a good night's sleep, we don't feel cognitively on game, our mood is affected, we feel lethargic, we don't have as much energy. But I'm not sure that most people realize the profound effect that even mild sleep restriction has on our metabolic health and glucose regulation. And this is extremely relevant because about one third of people in the United States do not meet the recommendations, which is seven to 9 hours of sleep per night for sleep. And again, this is very relevant for jet lag. I mean, there's a lot of relevance here for poor sleep. So mild sleep restriction, this is one to three fewer hours of sleep per night. So, I mean, one is not a lot. Doing that three nights in a row can increase fasting insulin levels. It can lead to higher insulin concentrations, elevated fasting leukagon levels, and also it decreases insulin sensitivity. Again, this is just getting 1 hour less of sleep a night for three nights. I mean, how many of us have probably even done that at this conference? Right? I mean, it's very easy and very applicable and it's having a profound effect on metabolism. Sleep debt is the cumulative effect of sleep restriction. Right. So this is when you're having multiple days of the sleep restriction. So in this case it was four, sorry, three days of 4 hours less sleep per night. That led to 40% slower glucose clearance, 30% decrease in glucose effectiveness. So this is independent of insulin, similar to diabetes, and 30% lower insulin response. So this is really indicating early diabetes. And these are in healthy people. These healthy people, after just three nights of having 4 hours less sleep a night, very profound effect on metabolism. There's been large meta analyses done on longitudinal studies looking at type two diabetes risk and sleep duration, and it's been identified that the optimal range of sleep for the lowest type two diabetes risk is seven to 9 hours of sleep a night. So going below 7 hours or above 9 hours were both associated with increased risk for type two diabetes. So the seven hour threshold, getting less than 7 hours of sleep a night, was associated with increases in fasting insulin, increases in glucose levels. Homo IR was elevated higher hba one c, and then also visceral fat was increased as well. So again, getting less than 7 hours of sleep a night, which a lot of people do routinely. And speaking of the elevated HBA One C, I think this is really important. Most of you probably realize this, but when you are constantly having elevations in blood glucose levels, this leads to advanced glycation end products, or ages, as they're called. And it's certainly a huge problem in people with type two diabetes because they are constantly having glucose dysregulation and they're elevated blood glucose levels. But generally speaking, when you have the hba one C high, you are talking about glucose reacting with lipids and proteins through the maillard reaction, including collagen. And this is all inside of our blood vessels, our arteries, you know, our myocardium making, you know, surrounding our heart. When you have those advanced vacation end products forming, it stiffens that collagen. Okay, HBA one C levels turn over after about, what, 120 days. Your collagen is in there forever. So what happens is you have those advanced glycation end products. If it's in your blood vessels, it stiffens the blood vessels, and this leads to hypertension. Plays a big role in hypertension. When it's happening in the arteries and in the myocardium, this decreases cardiovascular compliance, and it really plays a role in the stiffening of your heart with age. And so these advanced glycation end products increase the risk of cardiovascular disease, heart attacks, and hypertension. So having these elevations in your blood glucose levels and subsequently the hba one c biomarker, which biomarkers that is so much more than just type two diabetes risk, it's cardiovascular health, and it's really a cumulative effect that plays a role. As we age, there are a variety of mechanisms that have been identified for how short sleep and mild sleep restriction can cause dysfunctional metabolism. So we're going to talk about decreased insulin signaling and adipocytes. We're going to talk about lower beta cell sensitivity to glucose. We're going to talk about impaired glucose absorption in muscle and liver and then changes in satiety hormones. So there's been some studies looking at sleep restriction. This is about 4 hours of sleep a night for four days. It decreased insulin signaling and adipocytes by 30%. So, I mean, your adipose, your adipocytes are one of the major sinks, aside from muscle, for glucose disposal. Right? Storing. Storing it as fat, you know, for energy. But a 30% reduction in cellular insulin signaling adiposides is. I mean, you're talking about, these aren't healthy people. This is like a healthy person immediately becoming obese or immediately becoming type two diabetic after just four days. Right, of sleep restriction. So it's very profound in terms of metabolic health, sleep loss. So mild sleep loss, even, it does promote an obesogenic profile. And so a lot of work has been done out of Yves van Coucher's lab, and she's looked a lot at these hunger hormones, satiety hormones. So after two days of 4 hours less sleep, leptin levels go down. So people are not feeling satiated by their food, because leptin regulates satiation and their ghrelin levels increase. So it's a double whammy. Ghrelin is the hunger hormone. It tells you you're hungry. And so they're getting this continual hunger. So global hunger ratings go up, global appetite goes up. So people are not satiated by their food, and they're hungry throughout their day. And again, Eve van Kauter's work has shown that people eat more, and they're consuming foods and have cravings for processed foods, highly refined sugars, salty foods, processed fats, and fatty foods. So they're eating up to 45% more of those processed, unhealthy foods. And their hunger ratings are 24% higher. So they're eating even more than they would if they were getting a good night's sleep. So I think it's pretty clear that sleep restriction, poor sleep, does cause dysfunctional metabolism. And so the question is, can you fix your sleep and improve metabolic health? So there's a couple of evidence based ways we're going to talk about improving sleep. Both of them involve good sleep hygiene. So good sleep hygiene is really the foundation of good sleep. And there's a variety of factors that are, like, a checklist of it, and I didn't include all of them, but some of the main ones here are using light smartly. So bright light exposure first thing in the morning, at least 30 minutes, is one of the most important ways to reset your circadian rhythm so that you become sleepy at a normal time. Very, very important for resetting circadian rhythm, but also important for stopping that melatonin production when you're first waking up. Right. Also avoiding bright light, blue light exposure in the evening after sunset. Right. Blue light is what is inhibiting melatonin production in our eyes. It's through our eyes actually, not in our eyes, but it's inhibiting melanopsin, which then is involved in the signaling of producing melatonin to make us sleepy. You want to avoid blue light either by having light dimmers or different color lights, maybe red or orange. Also glasses you can wear to filter it out, but also realize that screens are full of bright light, blue light as well. Turning down the screens, maybe avoiding screens at night is another good idea. Also making sure your room is dark, because there's been studies showing that even a little bit of ambient light coming in disrupts sleep. Managing temperature is important. So part of what melatonin is doing besides making you sleepy is it's lowering your core body temperature. And this is part of the circadian rhythm. It's important for good sleep. And so you want to make sure you're not sleeping in a really hot room. And there's many ways that you can obviously maintain your bedroom temperature. Optimizing meal timing is also important. So in addition to the importance of avoiding eating, you know, like 3 hours before your bedtime because of melatonin production, it also improves your sleep. So this has actually been some work by Doctor Sachin panda at the Salk institute as well. He's identified from large studies that he's done that people that stop eating 3 hours, at least 3 hours before their bedtime sleep better. And that's also partially because you're not digesting. I mean, digesting is a lot of, it's an energy consuming process, right. That's happening while you sleep. So it makes sense that it would also disrupt sleep somewhat. Regular exercise. So again, these are all tied together. So the exercise is also a very powerful zeitgeber. So, you know, just routine exercise is also really important for resetting the circadian rhythm and helping you just get on that rhythm and go to bed at a normal time and then monitoring caffeine intake. Caffeine shifts the circadian clock by 45 minutes. So if you're drinking a cup of coffee, that's 45 minutes of a circadian shift, and then you have another cup of coffee, that's 45 minutes of a circadian shift, right. And so you're going to be going to bed hours later if you're doing, drinking four cups of coffee, particularly if it's, you know, afternoon. Obviously there's a lot of individual variation between the way we metabolize caffeine. So yeah, there's some individual variation, but generally speaking it still shifts circadian rhythm by about close to an hour. So sleep extension is one of the evidence based ways that's been shown to improve sleep. And this involves really just adjusting your bedtimes to increase the sleep time. So either going to bed earlier or sleeping in both of those. It also involves a lot of consultations with sleep experts and then sleep hygiene recommendations like we just discussed. And so there's been meta analyses looking at sleep extension in people that are short sleepers. So they're getting fewer than 7 hours of sleep per night. And when they undergo this type of behavioral change, when they're engaged in sleep extension for every hour additional that they're sleeping per night, they improve their insulin sensitivity. Regardless of their body weight, they improve and normalize their hormones, leptin and ghrelin, they have reduced appetite, right. They're not getting so hungry, their sugar intake goes down and their caloric reduction goes down and they lose weight. So all these things, of course, the sugar intake and reducing the calories, it's all regulated by the satiety hormones, which again, if you're increasing your sleep, you can basically flip that switch to kind of help regulate them back and normalize them back. The other type of evidence based way for improving sleep is a certain type of cognitive behavioral therapy for insomnia, CBTI. This is probably one of the most used, well known and effective ways to improve insomnia. It involves a variety of factors. I'm not going to go in depth on, but stimulus control is the main one. So that means the bed is only associated with sleep. So no watching tv in your bed, no scrolling on your phone, no doing anything, screens on your bed. That is for sleeping only. So that's stimulus control. It involves sleep restriction, which is a little ironic, paradoxical, but. So that means if you're laying in your bed and you're tossing and turning and you're up for an hour or two or three, it means getting out of your bed and going into another room, dark room like your living room couch and laying there and you do some relaxation techniques that you learn about and then wait till you get sleepy and then go back into the bed. So again, bed is for sleep only. It also involves implementing a variety of the sleep hygiene factors that we talked about. Sleep education and again, some relaxation techniques. So, meta analyses of CBTI have also been shown to improve metabolic health. People with insomnia, including improved HBA, one c, improved blood pressure, of course, their sleep quality and insomnia factors and all those things improve as well. So it's pretty clear that people that have poor sleep, that have insomnia, that are short sleepers, if they work on fixing their sleep, they improve their metabolic health. But there are situations where it is challenging to sleep longer, stay, you know, to sleep in, to do all these things, because maybe you're a new parent, right? And you have to wake up and your sleep will be compromised. There's absolutely nothing you can do because of it. There's other things as well, right? I mean, jet lag, things like that. So there is another way to improve metabolic health even when you're not sleeping optimal. And that takes. Takes us full circle back to the beginning of the talk with high intensity interval training. So, high intensity interval training has shown to be a very robust way to improve metabolic health when you are sleep restricted. So there's been studies that have shown that high intensity interval training, if you do three sessions over five days of also being sleep restricted, so sleeping 4 hours less a night, you can still improve your circadian rhythm, you can still improve your glucose tolerance, your mitochondrial function and biomarkers of mitochondrial function and mitochondrial biogenesis. And, you know, I mean, this is important because, again, the glucose regulation. So you're doing that high intensity interval training? Well, part of the way that that high intensity interval training, I mean, part of the way that sleep restriction impairs glucose regulation is it makes your muscle less responsive to glucose. And so what is high intensity interval training doing? It's doing the exact opposite, right? It's increasing glute, four transporters, and it's bringing the glucose into your muscles. So you're really countering some of that negative effect of poor sleep on your muscle, even doing high intensity level training before you know you're going to be sleep restricted. So I got on my peloton yesterday. I went hard right before I got on my flight from California. I knew I was going to lose some sleep because it's 3 hours ahead in Florida, doing high intensity training before you're going to be sleep restricted. Still mostly rescues the high blood glucose and acute insulin resistance that's caused by sleep restriction. So, yet again, just really important with respect to tools that we have at our disposal to help mitigate some of the effects of chronic sleep loss or even acute sleep loss, both a lot of those protocols, again, are the ones we've discussed. The tabata, the wingate conventional 1 minute on, 1 minute off and the norwegian four x four hit protocol. A lot of, a lot of HIIT protocols out there that people can do, or you just do your exercise snacks as well. I mean, that also has been shown to increase glucose homeostasis. As I mentioned, the ten bodyweight squats. And I do want to mention one last study before we end on time. And that is again, there's lots of data out there to be harvested from the UK Biobank data and there's been studies that have identified people that sleep fewer than 7 hours or greater than 9 hours a night have a higher all cause mortality. However, if those people are physically active and they're getting, and they're meeting the guidelines for physical activity, 75 minutes a week of intense vigorous exercise or 150 minutes a week of moderate intensity exercise, they do not have a higher all cause mortality. They have the same mortality risk as someone that's getting good sleep yet again. Exercise can forgive a lot of sins and there's no reason to not do a time efficient type of high intensity interval training workout. It's, you know, time efficient, it's easy exercise, snacks, I mean, there's all the evidence there. We just have to implement it, make it part of your hygiene. Like you brush your teeth every morning, you do your hit. So in conclusion, I think there's three really powerful tools we have to improve our metabolic health. I talked about the vigorous intensity exercise, high intensity interval training, making it part of your personal hygiene, also trying to eat your meals in accordance with your circadian rhythm. A good rule of thumb, stop eating 3 hours before bed. Because of that melatonin production. It's nice to have a pretty restricted time window, 810 hours and then also making sure we optimize our sleep and having good sleep. And that can be anything from the bright, you know, good sleep hygiene and all those things we talked about to people that have problems and doing things like CBTI or sleep extension. And certainly back to the exercise again to help. And with that, thank you so much for staying here and listening. Let me talk for an hour. I hope you guys enjoy the rest of the conference and thanks again.
Member only extras:
Learn more about the advantages of a premium membership by clicking below.
Get email updates with the latest curated healthspan research
Support our work

Every other week premium members receive a special edition newsletter that summarizes all of the latest healthspan research.