#8 Sleep, Daylight Anchoring, and Effects on Memory & Obesity with Dan Pardi
This episode is available in a convenient podcast format.
These episodes make great companion listening for a long drive.
The BDNF Protocol Guide
An essential checklist for cognitive longevity — filled with specific exercise, heat stress, and omega-3 protocols for boosting BDNF. Enter your email, and we'll deliver it straight to your inbox.
Dan Pardi is a Ph.D candidate that researches sleep neurobiology at Stanford and University of Leiden. He is also co-founder of Dan’s Plan, an online wellness and technology company. In this podcast Rhonda and Dan discuss what the determinants of good sleep are including duration, timing and intensity, the major causes of less sleep in our society, the consequences of sleep loss including decreased purging of toxic substances from the brain, damage to neurons that signal to the brain to stay awake (and how this leads to that feeling that you need coffee in the morning), increased incidence of chronic diseases such as cancer and type 2 diabetes, cognitive and behavioral impairments, the impact on eating behaviors and weight gain. We also discuss what the optimal amount of sleep is, the importance of sleep timing, and keeping the same schedule as well as other ways to improve sleep.
-
What is the circadian rhythm and how is sleep relevant for our health.
-
Lack of light is required to regulate melatonin production and communicate with the suprachiasmatic nucleus to regulate circadian rhythm.
-
Lack of sleep causes a 4-fold increase of cancer risk.
-
-
-
Dan Pardi explains how all 4 phases of sleep are important for overall health.
-
Sleep deprivation will increase appetite and decrease energy expenditure through the hormones leptin and ghrelin.
-
Sleep deprivation increases brain reward response and which increases likelihood obesity and theoretically addiction.
-
Dan Pardi explains how sleep is critical for transfer of short-term memory into long-term memory.
-
Sleep and wake are triggered by a dynamic interplay of sleep pressure and wake network.
-
-
-
Dan Pardi explains good practices for getting enough sleep and how much sleep is ideal.
-
As sleep deprivation grows, decision-making is more erratic and risky.
-
Under ideal conditions, a person can shift their circadian rhythm by up to 3 hours a day.
-
Review of practices that encourage a healthy sleep life and effective circadian rhythm.
-
Correlation of healthy diet and proper sleep & study suggesting DHA improves sleep quality in children.
-
Dan’s plan (aka HumanOS) is bridging the gap between what we know in science and what you can do to improve your personal health.
-
Dan Pardi’s recent publication: Eating Decisions Based on Alertness Levels After a Single Night of Sleep Manipulation: A Randomized Clinical Trial
- Rhonda: Dr. Rhonda Patrick here. Today I'm excited to be sitting with my friend, Dan Pardi. Dan is a soon-to-be PHD. He researches sleep neurobiology at Stanford University and also at the Leiden University. I know you guys are all a bunch of sleepyheads, so I think that Dan, why don't you tell us a little bit about sleep?
- Dan: It is a topic near and dear to my heart. Yeah, so I got into sleep probably 12 years ago, and it was very serendipitous. There was a job opportunity for a place called Orphan Medical, and it's a pharmaceutical company that was working with the FDA to develop drugs for orphan disorders, which are usually considered disorders with 200,000 people or less. So they're not populations that are large enough to get large pharmaceutical companies to develop medications for them. So Orphan was looking at how to develop drugs for these populations. Narcolepsy, which is a sleep disorder, was on the radar. So they had a medication, sodium oxybate, or GHB, and they were hiring. I applied for the job, and I knew nothing about sleep, narcolepsy, or sodium oxybate before I started. And it was a very fortunate experience for me, because as soon as I started to understand more about sleep, it's just a window into our world that's so important, it's so interesting, and it's truly one of these topics where the more you learn, the more you want to know.
- Rhonda: Absolutely. I am convinced that sleep is one of the key determinants of health, both performance and the way we age, and it's regulating a lot of things. If you could talk a little bit about the circadian rhythm, and how that's connected to sleep and why that's so important.
- Dan: Yeah. So that's a great point. So, sleep is a circadian rhythm, and what a circadian rhythm is is a repeatable, 24-hour process that usually we have cyclic activity for things like behavior, for cell cycle growth and repair processes for all different activities in the body. The timing of these rhythms are dependent on basically this system in the brain called the suprachiasmatic nucleus, which is synchronizing with the light-dark cycle of the environment. And so, then, we have what are called clock cells within every tissue and cell in our body. And so there's basically two levels of synchronization that are taking place; the master clock in the brain, with the light-dark cycle of the environment, and then all the cells in our tissues with the master clock. And that keeps our body in-time, so it's doing a right behavior at the right time of day.
- Rhonda: Yeah. I think, if I'll just add on here, the thing that's, to me, so striking is that these circadian rhythms, you say they run on the day-night cycle or the light-dark cycle, over 15% of the human encoding genome is regulated by the circadian rhythm, and what that means is that genes are being turned on, so they're active and doing what they're supposed to do during a function, or they're being turned off so that they're not active, according to this rhythm. So you're talking about a huge amount of metabolic processes, behavioral processes, all these different processes that are controlled.
- Dan: That's right, and that's why there's really no part of the body that goes untouched when we're not getting good sleep, or when we have mistimed circadian rhythms from what are called aberrant light environments, or we're getting weird, funky light environments that our bodies are not used to, in terms of our physiology. And so that is actually pretty descriptive of the modern world. We spend 90% of our time indoors. Two-hundred years ago, 90% of the population was working in agrarian capacity, outdoors, all day long. In the evening, we can turn on artificial light, and we can watch high-definition screens, and we can use our e-readers, and all of these are emitting light, and our brains are trying to figure out, "What time of day is it?" And because of that strange lighting environment, instead of having this waxing and waning of activity controlled by circadian clocks, then we have what's called asynchronization, where there's not really a robust message that, "Hey, it's daytime. Do daytime activities," and, "It's nighttime. Do nighttime activities." And I think we're running a huge experiment with our biology right now, and the outcomes are probably not going to be very favorable. And we know that already, through looking at people that have chronic sleep disorders where they have disrupted sleep, or shift workers, where they're working during the day sometimes a week, and during the night other times a week. We see that when you don't have good sleep, and when you have highly fluctuating or highly variable periods where you're sleeping, and therefore mistimed circadian rhythms, that you have really four-fold increases in cancer risk, you have multi-fold increases in risk for diabetes and for metabolic syndrome, cardiovascular disease. It's not a nice-to-have, it's a must-have.
- Rhonda: Right. Let's dive into that a little bit. So I know, with the cancer, for example. The cancer incidents I've become particularly interested in with sleep, the connection between lack of sleep and cancer, and one thing in particular, you're talking about the suprachiasmatic nucleus and the sensing of light, I know that one hormone involving that is melatonin, right?
- Dan: That's right.
- Rhonda: And you mentioned something about exposure to light at night and things like that, so that's messing up our melatonin. Correct?
- Dan: Yeah, that's right. I'll tell you about how it's produced, and I bet you can tell me a lot more about how that works then in the body. There are these cells in the back of the eye that are called retinal ganglion cells, and they were discovered in the mid-90s, and they act almost like rods and cones do, which detect light...excuse me. They're looking at light to detect color and light intensity, and then they can transduce a light signal into a nerve signal. Now, when rods and cones are triggered in that way, that message goes back to the primary visual cortex, where we turn light into image. In the mid-90s though, a different type of cell that previously had not been discovered was identified by a researcher, Ignacio Provencio, and he found that okay, there's another retinal ganglion cell that can also do this, it can also turn light into a nerve signal, but that nerve signal's not going back to what's called the suprachiasmatic nucleus, or the master clock. And that was a very important discovery. So anyway, when melatonin is produced under something called "dim light melatonin onset," when the light dims in intensity, and also the tone of the light changes, or the color of the light changes, then melatonin is produced in the pineal gland, this multisynaptic loop. So it is the perception of light by the eye which is eventually the trigger to say, "Okay. It's becoming dark. Produce melatonin." And then melatonin, we think of that as a sleepiness hormone, but it has fairly weak soporific activity, which means it's not a very strong stimulator for sleep, but it's more of a reinforcer that it is in fact dark out. And so it's telling all the clocks within the suprachiasmatic nucleus, "Yeah, it's now nighttime. Do nighttime activities." So it will affect the transcription and the translation activity that's happening.
- Rhonda: One thing that you might find really interesting is that, you're talking about this discovery back in the 90s; recently, they discovered, in some sort of aquatic organism, I think it was like flagella, or some dinoflagellate, or something. I don't recall what specifically the organism was. But they produce melatonin, and the melatonin that they produce regulates them swimming up and down. And I thought that was so fascinating, because it's just so evolutionary conserved that it's like being produced in these little, tiny sea creatures. But back to the melatonin, the functions, it's a hormone, and it controls over 500 genes in the body, and as you mentioned, it's shutting down certain metabolic processes, and the shutdown of those processes are important for other ones to be turned on at certain times, so it's very important for regulating metabolism. But what's also really interesting, to bring it back to the cancer that you mentioned, you mentioned there was like a four-fold increase in cancer incidents with lack of sleep. And that's so interesting, because there's been a couple of studies recently that have shown, for example in mice, when you engineer them to get breast cancer. You probably have seen this study. And these mice, when they're exposed to light during their nighttime cycle, they are resistant to traditional chemotherapeutic treatment, so the breast cancer cells won't die. But, if you expose them to this pure darkness, the cancer cells become sensitive to death. And what's interesting is that, this is something in people, there's been for example, blind people, who are blind, they actually make more melatonin, and they have twice less cancer incidents than people that are not blind. There has been studies that have been done with supplemental melatonin in breast cancer patients, two small clinical trials I've seen. There's been other cancer studies as well, but they're given them really high doses of melatonin, and in conjunction with other traditional therapies like radiation, it increases, like, the one-year survival rate from 36% to, like, 65%, or something like that.
- Dan: Fantastic.
- Rhonda: So it's really interesting, this link between melatonin and cancer. And if you look closely at some of the genes melatonin regulates, angiogenesis, which is the growth of new blood vessels, which is how cancer cells metastatize and spread, it regulates natural killer cells, which are important for killing cancer cells. So very important in cancer. But some of the other things you had mentioned in a conversation that we've had before is the role of sleep in, since we're talking about diseases, clearing out toxic substances in the brain.
- Dan: This is a very interesting and hot subject right now. There's been two pretty major studies that have come out, one in 2013, which was looking at something called beta-amyloid, which is this potentially toxic protein, that we believe is involved in Alzheimer's disease. There's one study that came out that showed that during sleep, the space between neurons expands, and that gives room for this goopy substance to actually get out of cells and get cleared by the cerebral spinal fluid. So the brain goes through this power cleanse in the evening, and it might be one of the major functions of sleep. The more recent paper out of Berkeley, by Matt Walker's lab, or he was on the paper. I'm not sure if his lab did it. They showed that this beta-amyloid protein, particularly when it clusters in a part of the brain called the medial prefrontal cortex, then that will suppress the generation of something called a type of[SP] slow wave sleep. So maybe I'll pause and I'll just mention the different stages of sleep real quick to give a little context. So when we go to sleep, generating sleep is an active process by the brain, and you go through different sleep stages. So you'll have non-REM, and out of non-REM you'll have stage one, stage two, and then what's called slow wave sleep. And then you will switch over into what's called paradoxical sleep or REM sleep, and you will go through five of those cycles over the course of the night. It's funny, because I get questioned a lot because of the work that I do, evangelizing the importance of sleep. People are always wanting to know, "What's the important stage of sleep?," and really, they're all important. They're all doing something that's really critical for the brain and body to restore itself. So this study in particular showed that this area of the brain that I mentioned previously, the medical prefrontal cortex, it's very important for generating a type of slow wave sleep that then is important for clearing out beta-amyloid. And so if you're not generating a lot of that type of sleep, then you're going to have an accumulation of beta-amyloid. And conversely, if you have a lot of beta-amyloid, it's going to suppress that type of sleep.
- Rhonda: It's a feedback loop.
- Dan: It is.
- Rhonda: Wow, that's really cool. I didn't read that study, but I remember seeing the headline, the second. The glymphatic system, which is what Dan was referring to when he was talking about how cerebral spinal fluid squirts up through the brain, washes out all the toxic substances, including amyloid-beta, which aggregates outside of neurons and is thought to play a role in disrupting synapses, the connection between neurons and things like that, is really important. Your brain swells. It literally swells, at least in rats or mice, they swell. It's extremely important, because that's one of the major ways that we can clear amyloid-beta plaques from our brains, and so that sleep becomes just so critical. Not to mention you're repairing damage when you sleep. DNA repair, enzymes, antioxidant enzymes. These are all being turned on, some of them by melatonin, some of them by possibly other circadian rhythm genes, but those are being turned on during sleep. So it's just so important to take the garbage out, to repair the damage we've done throughout the day, you know, things like that. I know, personally, like when I don't sleep, while I'm more susceptible to like...anything inflammatory that's going on is exacerbated. And that's very interesting. There's some other studies, I don't know if you've seen, pointing to, for example, the guy. There's bacteria in our gut are also on a circadian rhythm.
- Dan: Yeah.
- Rhonda: Crazy. So when our sleep is disrupted, these bacterias, their circadian rhythm is also disrupted, and that affects metabolism, it affects the way they're metabolizing foods and things like that. You also mentioned type 2 diabetes and obesity. Can you talk a little bit about mechanisms for how sleep...
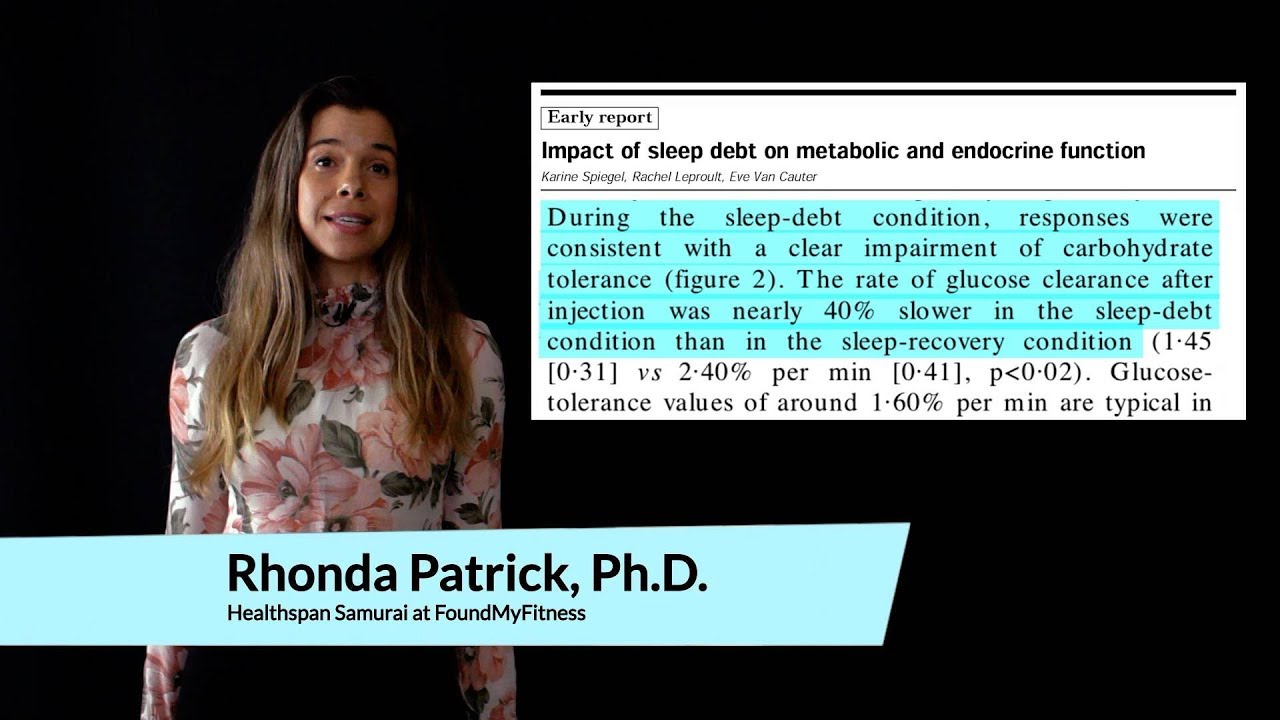
- Dan: Sure. This is an area that I do my work in, and I'd say that this subject became pretty hot probably 10-15 years ago. And it started when people were doing sleep deprivation studies, and they were looking at blood glucose levels, and they found that, by either getting inadequate sleep, so not a complete night, or total sleep deprivation, that people were looking pre-diabetic, where before, they were not. And so you'd have this profile of regulating blood glucose. If this was tested, that seemed that you were just in a different place in your life, because they would start with young, healthy adults, and then all of a sudden, after one night of sleep loss, they would look like they were pre-diabetic. So that finding, which was fairly serendipitous, stimulated a whole line of research. After that, the next area of exploration was looking at all sorts of metabolic hormones, hormones that are involved in the regulation of energy expenditure or hunger. And these are things like leptin, which is released from fat tissue, and is a signal to the brain of how much fat we're storing on our body. Also, another hormone called ghrelin, which is released by oxyntic cells in the stomach. And that's a fascinating hormone, because it does quite a lot of things, but it's the only gut-derived hormone that will actually stimulate hunger. Must gut-derived peptides are actually in response to a meal and they stimulate satiety[SP]. So this hormone, ghrelin, actually will episodically, which means over the course of the day, its own activity will wax and wane. It's low after a meal, but it will gradually rise, and that is going to stimulate hunger. And what they found, after sleep loss, is that leptin levels were lower and that ghrelin levels were higher. And without getting into too much detail, that profile would mean that you're going to be hungrier and you're going to have less energy expenditure the next day.
- Rhonda: Wow.
- Dan: Yeah. So that was really exciting.
- Rhonda: That's a pretty big consequence. It also tells you that you probably, if you're going to get your blood tested by your doctor, whoever, probably do it more than once. Because if you go and do it after a terrible night's sleep, you might look like you're insulin-positioned[SP] or pre-diabetic, right?
- Dan: Absolutely.
- Rhonda: That would be kind of terrifying. What about the effects of loss of sleep. We're talking about obesity, type two diabetes, and these hormones related to satiety and hunger; what about those hormones or neurotransmitters related to reward or food reward?
- Dan: Yeah. It's a great question because, as that line of research evolved, basically there were several things that became of interest to understand this association between sleep loss and obesity that seemed to be present. So at one point, it was a couple years ago, but I had a slide on a presentation that was 81 out of 89 studies, epidemiological or longitudinal studies, that looked for an association between sleep loss and weight gain had a positive finding. So you had a 55% risk increase for obesity if you were getting less than six hours of sleep per night. So there was like, "Okay, something's there, but what's going on?" And actually, when you looked further into this hormone regulation by the body, and I've actually published one study in narcoleptics and ghrelin, and we didn't find that there was any difference. And so I know that literature pretty well, because some early findings showed, "Wow, there's really something going on here," but then subsequent findings didn't show that there was a change. And so, it was equivocal. Sometimes it said there seemed[SP] that there was something going on, other times there wasn't. Whether not one side of that is wrong, or there was something else happening, like a lot of things in science, always good to repeat the study, right? But the next kind of hot thing became, because fMRI became more broad in terms of its usage, we started to look at the brains of sleep-deprived people and how they would function after sleep loss, and particularly after sleep loss in response to palatable foods, foods that we know that we really like a lot, but may not be so good for us.
- Rhonda: Like junk food?
- Dan: Like junk food. Yeah, exactly. This is usually energy-dense foods. A doughnut could be another example, or ice cream, stuff that we really do think is very tasty, and the response that our brains have to those foods that we like is elevated, so that if you were to look at things like, for example, the activity of certain areas that process hedonic stimuli, what that means is areas that light up to pleasurable stimuli, they would light up like a Christmas tree after sleep loss.
- Rhonda: Wow. So your brain basically, your...okay, so there's two things I'm thinking. One, that your reward center is hyperactive, so you're of course eating some terrible food, and then you're getting this major reward from it. But the second thing is, what about addictive behavior, and if you think about most people that have insomnia, for example, they go to the doctor and they say, "Doc, I can't sleep. I have insomnia. What can I do?" and the first sort of thing the doctor says is, "Here's this drug, this prescription pill," whether it's like Ambien or some other sleeping pill, "This may help you sleep." That may actually be a terrible thing for someone who's already, their brain chemistry is a little off because they're not getting sleep and so their reward circuitry is all screwed up. Now they take this sleeping pill; they may become more addicted to that sleeping pill, theoretically.
- Dan: That's interesting. Yeah. I hadn't actually ever thought about that. It's interesting to think, whenever you're doing science, it's easier to study the short-term effects of things, but then it's harder to study the effects of persistent, chronic exposure to whatever that situation is. There's something called the allostasis, which is a type of stress response that can happen over longer term exposure. Is there a favorable kind of adaptation or acclimation that the body makes through repeated exposure to certain things, where maybe you would have a blunted response to these sorts of foods if you're always sleep-deprived? I don't know. This is kind of speculation [inaudible 00:23:27].
- Rhonda: I'm so glad you brought this up, because we've been talking a lot about some of the consequences of sleep loss, so you mentioned obesity and type two diabetes, Alzheimer's disease, because the glymphatic system, if you're not sleeping, you're not clearing out the amyloid-beta plaques. Cancer, you mentioned. Brain atrophy is another one, right? Learning and memory problems, I guess. There's a couple of studies I've seen. In fact, I've seen you share one study that I found particularly interesting, was sleep, during sleep, I don't know what part of sleep it was, but oligodendrocytes...no, it was dendritic spines reproduce, and they help form synapses or something, and this happens after you learn something, or like an episodic memory occurs, or you're doing something where you're learning through an event, and then you go to sleep, you make these dendritic spines, and they're somehow finalizing the synapses or something like that. Anyway. So I found that was very interesting, and I remembered you shared that study.
- Dan: I can share a little more about it.
- Rhonda: Awesome.
- Dan: So this is, basically, to kind of summarize my research a little bit, after wanting to understand more about how the body responds to sleep loss, particularly related to food decisions and obesity, I was also very interested then to understand, "Well, what are the cognitive effects of sleep loss, including learning and memory?" And so during the day, like for example right now, you're listening to this message and your synapses are getting challenged and stimulated, and that is going to cause kind of a modification of them. At night, you're going to have two things that are going to then facilitate a consolidation of that memory, which means it's going to then make it stronger. Your brain is going to replay that activity pattern in a very selective use pattern.
- Rhonda: Wow.
- Dan: Yeah. So if you use that part of the brain, that part of the brain at night is going to be replayed.
- Rhonda: Isn't there a chemical, like 4BP-something, that you produce that's like involved in that? I remember reading a paper...
- Dan: There's several. Yeah. So the key aspects are NMDA receptors, and then protein kinase A. So if you block protein kinase A, then you will not have any long-term transformation of hippocampal memories, which are what you kind of...it's where memories go during the day when you're learning, over to more cortical areas at night, where then those memories, they move. They move from the hippocampus to the cortex. And you don't have that transformation if you basically get sleep deprivation, or if you block NMDA receptors. And what ends up happening is, usually you see a real enhancement of declarative memory, which is the learning of certain types of facts. It's two types of long-term memory. You basically see a suppression of that. So usually, you might see an increase in 20%, in terms of memory retention after, say, you were to study a list of words. You'd have 20% improvement in performance the next day after sleep. Without good sleep, or blocking these NMDA receptors, you're not going to see any of that benefit.
- Rhonda: Wow. What about GABA? What about the GABA system in the process you were talking about, where you're reliving the memory or the experience you just had? Does GABA play a role in that?
- Dan: So GABA plays, it's a critical role, as it's the major inhibitory neurotransmitter in the brain. The way that the cortex...there's a good way to think about sleep, is there is a system, it's not one monolithic kind of system that's waxing and waning, but you actually have a wake network, which is a clustering of different nerve cells. So you've got, for example...
- Rhonda: A wake network?
- Dan: A wake network, yeah. So you've got a group of cells in the basal forebrain that use glutamine to activate the cortex. You've got a group of neurons in the dorsal raphe, which is a part of the brain that produces all sertogonergic cells or serotonin producing cells that is activating the cortex. You've got an area in the locus coeruleus...you could name a bunch of these that are all involved in activating the cortex, and those are orchestrated, or basically they're coordinated by one group in the area called the hypothalamus, that produces hypocretin cells. And the reason I know about this pretty well is because people that have narcolepsy are missing these neurons.
- Rhonda: So what are they doing?
- Dan: So hypocretin, a good way to think about hypocretin is that it's a symphony conductor, and it is telling the wake network, "Hey, it's daytime. Be on. Play. And not only play, but play at a certain volume." And the reason not only it's giving like two levels of messaging, "Play and play at this level," is because the wake network is always acting proportional to how much sleep pressure you've built up. Sleep pressure is something that builds from the moment you wake up, and it keeps building, building, building, until you go to sleep, and the wake network is counteracting that all day long. And at the end of the day, the wake network goes to sleep, or turns off, and then you've got all this unopposed sleep pressure, and that will initiate sleep and keep you asleep for the rest of the night, so consolidated as well. So that's kind of that dance that's going on during the day, behind the scenes. And at night, the activity of GABA will activate in one area that is...it's funny. Parts of the brain become more active at night than at any other part during a 24 hour period, and one of those areas is called the ventrolateral preoptic area. It turns on to turn off the wake network, and that's what is enabling you then to kind of get overcome by the feeling of sleepiness, and then that's why you feel sleepy and fall asleep and stay asleep.
- Rhonda: So what happens when you are not getting sleep? Let's say you have insomnia, and we can talk about some of the causes of these sleep problems later, but what happens to that sleep network then? Or, sorry, the wake network.
- Dan: Yeah. The wake network, the timing of the wake network is off, all right? It has shifted. And so, what ends up happening is that you have an under-alerted brain for most of the day, because of artificial light, because of the lighting environment, which is the first thing we talked about. Because we are getting too much light at night, it is telling our brain that it is daytime, and that causes our circadian rhythms to shift. A good way to think about how these circadian rhythms shift is, let's say you were to go from, we're in San Francisco right now, and if you were to take a plane and you were to go to Italy, when we arrived, our biological time would be still set to San Francisco. But over the course of five, seven days, because of light entering into our eye at a time that's appropriate for Italy, our own biology would shift to match that environmental pattern. Okay. So that's kind of a good way to think of it, because we all usually can understand, yeah, it takes a while to adjust to a new time zone. Well, we're basically putting ourselves in mini-jetlag when we do this and by living in this manner, where we're getting not enough light during the day, and we're getting too much at night. And what that does, our brain thinks that it's daytime later than it should, and that shifts our alertness rhythm, and there's two consequences to that. It means that, because it's shifted, our wake rhythm is starting too late in the day the next day, and that means it's going to be kind of under-stimulated during the day, our brain is not going to have enough of that wake drive. And so therefore we need coffee, right?
- Rhonda: I was going to say, that's why you wake up and you feel like you need coffee.
- Dan: Totally. And then at night, it's over-active, because it's this kind of cyclic activity. And so now you want to go to bed, I mean, I'm sure people are going to have experienced this; "I was sleepy all day, and then right before bed, I woke up and I felt more alert than I did all day, and I couldn't sleep." And that is, again, characteristic of a normally functioning body in an abnormal environment. So we're getting signals that our body is responding to appropriately, but it leads to inappropriate physiology, as well.
- Rhonda: Why don't people that live in like Alaska or Norway, where it's like the daylight is all crazy at certain points, has there been any research on their circadian rhythm or are there polymorphisms they have that adapt them to that? Do you know?
- Dan: You know, I don't know about that, but I know that a colleague of mine did some work at the Concordia Bay[SP] Station in Antarctica, and the reason you would do that is if you're looking at the importance of light on health, it's great to go to a place like that where there's zero light for certain times of year, so you can study the effects of artificial light only on human physiology. And what they found is they had people in the space[SP] station that were living under normal room light, and what they found is that their mood was altered, they wanted to go to bed a little bit later every night, they didn't have a good anchored rhythm, and their reaction time on something called a "psychomotor vigilance test," which is a measurement of alertness, which the way that you can think about that is it's how energized the brain feels. Basically, they were performing very poorly. And then when they put in blue-enriched white light, when they replaced normal light with blue-enriched white light, everything improved. Their reaction time was better, their mood was better. And they went two weeks with normal light, two weeks with blue light, two weeks with normal light. They kept switching, and every time they would switch back and forth, they would notice that there was either really good effects or really bad effects, and it just speaks to the importance of having the right type of light.
- Rhonda: So bright light shuts off melatonin, the blue light, right?
- Dan: Yeah. You want a lot of it during the day, and then you don't want too much of it at night. Yeah.
- Rhonda: Talking about some of the causes of sleep problems, you were mentioning that being a major one, what about...I know for me, if I drink coffee late in the day...I actually drink mostly tea, so I drink coffee maybe one to two days a week, because there are some benefits I like from the coffee. If I'm having an interview, I'll drink coffee, so I'm all pumped up. I'm a little more sensitive to it. But one of the things that really affects me personally in terms of sleep is negative thoughts, things that are causing anxiety. If I have a problem I haven't solved or addressed, that can keep me up all night. And that's something that I'm sure a lot of people relate to. Everyone's probably experienced that.
- Dan: Totally. Everybody.
- Rhonda: But things that can help overcome that, obviously dealing with the problem...what about like meditation, being mindful?
- Dan: Yeah. So give a little context to this. We talked about that a little bit ago, is there's basically two different systems that are controlling how alert or how sleepy you feel at any point during the day. And one of them is this pressure for sleep and the other one is this wake drive, which is counteracting it. But then there are other modulators, too, which is social interaction, which is urgency of situation. And so those things can activate other resources that can then further activate the brain. So people that are experiencing, for example, post-traumatic stress, they have an overactive fear center, which is in the amygdala. And you have, I don't want this to be too much of a neuroanatomy lesson, but earlier, we talked about the medial prefrontal cortex, and that actually talks to the amygdala. That part of the brain, remember, is the part that's generating that really important slow wave activity which is then clearing out beta-amyloid. The amygdala is a fear center, and what happens if we are ruminating on something that was perhaps really horrible that we saw or that happened to us, that can then suppress the activity of this medial prefrontal cortex. Additionally...
- Rhonda: Interesting.
- Dan: ...what that amygdala can do is it can directly activate parts of the wake network, like the locus coeruleus.
- Rhonda: Wow.
- Dan: So what ends up happening is people that have post-traumatic stress - or it could be any sort of a stress, or it could be a love lost, it could be stress at work, it's a lot of things - it can interfere with sleep in a very significant way. And the really crappy thing about that is that when you don't sleep well, you worry about your sleep.
- Rhonda: It's a vicious cycle. When you're not sleeping well, you're more emotional, you're more stressed.
- Dan: Worried.
- Rhonda: And so it's like this horrible feedback loop.
- Dan: Yeah. It's rough.
- Rhonda: There was an interesting study that was done...where was it? I don't remember where it was done. I think it was published 2014 or 2013. You may have seen this, but it was interesting because most people associate exercise with being able to sleep better. It seems like if you're thinking about basic mechanisms, it seems logical. You're stressing your body, you're stressing your mind, you're going to sleep better to recover from that, I guess. But what was interesting is that there was a study, and there's been a lot of associative studies saying exercise is associated with improved sleep, but this particular study that I remember was interesting to me because it was done on women that had insomnia, and they were sedentary. So they didn't exercise, they had insomnia, they went for treatment, so were part of this controlled trial where they were then prescribed exercise. It was like 30 minutes a day for, I don't remember how long, I think it was like a few months. But the interesting thing from the study was that, so they did like an acute dose, like once or twice or a few times, and that did not make them sleep better. It actually exacerbated their sleep problems. But it wasn't until, and you mentioned this earlier, the repeated response and how you have feedback loops happening, so it wasn't until they had exercised for like a few months that they were able to really have significant improvements in sleep. And so, if you think about it, if you're a stressed person, if you're emotional, if these things things are causing sleep disturbances, and you exercise, continually exercise, then you start to sort of dial back some of that arousal of emotional centers[SP]. It's kind of funny, because my mom has sleep problems, and I've been telling her about exercise, and she'll do it like once, and then it has no effect, and she gives up. So really, the bottom line here is, don't give up. You need a routine. You need a training program. I don't know if you know anything about the types of exercise, or if there's been any studies showing different types affect sleep differently.
- Dan: Yeah. Early on, in the '70s and '80s, when we were just trying to understand some of the fundamentals, it was presumed that exercise had a favorable effect on sleep, and the investigation into that, the early investigations, didn't actually show that there was really much of a connection at all. Later though, and I wish I knew this well enough to describe what the differences were between the studies, a friend of mine, Matt Beuman[SP], who is on a paper that we're about to submit for some of my research, which we kind of talked around a little bit earlier, but he's actually done quite a bit of work looking at, "Does good sleep help you maintain a physical activity program, and does a regular physical activity program help you get good sleep?" And basically he's published several different papers that have looked at that kind of idea different ways, and you see that kind of directionality, there. So good sleep helps you be a physically active person, and being physically active helps you sleep well. Both sleep and exercise are a fundamental part...again, they're not nice-to-haves, they're need-to-haves, to have our body work well. And now we're, in a lot of ways, trying to just play catch-up, or we're trying to figure out, "What is the minimal dose that I need to perform well? Because my job really requires that I sit at my desk all day." It's such a frustrating thing, but I think life is going to be a lot different 15-20 years from now, because there's already real significant awareness. Environments are changing at work, people are using standing desks, even treadmill desks. I think that in the future, when we go to work, we're going to be doing physical work and our mental work. There's an understanding that daytime physical work is going to stimulate a good, positive mental state that will help get work done, and it's also going to help you sleep well. I think that environments and cultures, environments will be designed and cultures will be designed for keeping the person healthy, and that will help keep the person productive.
- Rhonda: That would be awesome.
- Dan: I would love that, and I'm on that mission.
- Rhonda: Totally.
- Dan: I'm really trying to help promote that.
- Rhonda: So what do you think is the optimal amount of sleep? I've seen several studies showing different factors. What are your thoughts on optimal sleep and how...
- Dan: So I like to promote...so the determinants of good sleep are timing, intensity and duration. So duration is easy, and that's like, "Well, how much sleep do I need?" and that's the one that most people go to readily, "How much time should I spend in bed?" That's one important component. That one is really dependent on you, and it changes across the lifespan, and it can also change on whether you're fighting an infection, or doing really intense physical activity; you might need more than your average. So you're going to have some night-by-night variation. What I like to do in order to get enough time in bed, I let my body determine how much sleep I want, so I try to give myself a little more time in bed, for the amount of sleep I expect to get. So let's say I usually get eight hours, I try to be in bed for eight and a half. And yeah, maybe I'll wake up not by an alarm clock, by external means, but by my body waking up. I always want that to be the case. So the alarm clock is kind of like the stopgap, like I really can't sleep in beyond that, but I'm trying to plan enough time in bed so that I don't actually need it.
- Rhonda: That's awesome. That's kind of what I do. I most of the don't use an alarm, but it's there programmed as a fail-safe, like, "Okay, if I don't get up, if I have to be somewhere and I have to get up." But I think that's a really great bit of information, is to give yourself more time, and that probably means getting into bed earlier, right?
- Dan: It does, and that's kind of the hard part, because we, as work times extend and the work permeates into our life, because we've got the ubiquity of devices that make, you know, there's no boundaries anymore to work. It follows us everywhere we go. So if you're in a culture where you're getting emails really late at night, it can make it really difficult. And if you're in position where, let's say, a boss is sending you emails, it might be hard to say, "All right, I'm just gonna turn it off and pay attention to it in the morning," but it's also good to be able to do that. So anyway, I try to do exactly what you do, so I focus on getting into bed at a certain time every night, and that keeps it really simple, and I know I want to be in bed by 11, and that's easy, you know? And I know, unless my time that I need to wake up changes, then I basically work backwards from the time I think I need, and that's my time to be in bed.
- Rhonda: Yeah. The other thing is, something that I do is I, because as you talked about, we talked in the beginning how important light exposure is at the right times, and not having a lot of exposure at night. I've got these Philip Hues lights that are orange light, and I have them in the house, and so those go on at night. And then I also have an app on my computer screen, because we don't have a TV, Dan and I watch movies from a computer screen. So then we've got this app that filters out the blue light, so try to kind of minimize the amount of blue light. I have a hard time with the emails because I'm answering them. But that's my biggest thing I need to work on, because you will, you'll get emotional. And being emotional about something, even like good emotion, like I'm excited, whatever, it doesn't matter, just emotional, I have a hard time getting to sleep.
- Dan: Yeah. Under sleep deprivation, and also during stress, emotions are heightened. So if it's negative, it's more negative, if it's positive, it's more positive. Pain, you have a greater sensitivity to pain. There's just kind of a heightening...I know that pain is not an emotion, but there's just a heightening of sensitivity.
- Rhonda: So everyone should sleep.
- Dan: Yeah, exactly. Interestingly, and this is going to sound contradictory to what I've been saying so far, but a lot of creative thinkers and artists, like if you think about when are a lot of albums made, they're made late into the night. And there's an untethering of...so there's something called the neuro-competitive model for decision-making, and if you think about how the brain works is that you have this impulsive brain that is just like saying yes to things that it finds pleasurable, and then there's an editorial component, which is in the frontal cortex, and it's saying, "You know, maybe that's not such a good idea. Maybe you shouldn't have a doughnut, more or less than 12." And so, depending on which part of the brain wins out, it's going to determine the behavior that follows. What I didn't mention previously, during sleep deprivation, not only do you have heightened emotional reactivity, but you also have suppressed cognitive control. So those areas of the brain are basically like offline. Yeah. So you have what's called a shift in your economic preferences, which means that you're going to be more likely to, if you're gambling, you'll be like, "All right! Put it all on black!" You're going to take larger risk and you're going to take more frequent risk.
- Rhonda: And you're going to get rewarded, I mean, you're going to have that rewarding going on more for those, right?
- Dan: Yeah.
- Rhonda: Like the doughnuts, you're going to eat more doughnuts. Anyways, it sounds like sleep, there's so many different lifestyle factors that it's affecting. It's been associated with shorter telomeres, aging, neurodegenerative disease, cancer, obesity, emotional arousal, what else did we say? Addiction.
- Dan: Yeah. It's...
- Rhonda: Endless.
- Dan: It is. It's that fundamental part of our physiology, and it's a need-to-have, not a nice-to-have. So when I speak about sleep, I'm always interested to show the connections, so that people will kind of escalate its value, because it comes down to the decision, the actual practical decision is, "Oh, one more episode of Game of Thrones," right? It's something that you really want to do, and you're already in this state where you're more likely to just say yes to that. The point that I didn't make clearly earlier is that, as work kind of gets into our life, we're always going to try to fight for a little bit of personal time, and that oftentimes means that sleep is suffering. So knowing some of these connections, whether you could repeat these back or not, that's not important. You know that it's important. Now it's kind of on you to say "Okay, I need to then create what I call a "sleep practice"," which just means, "All right, what are the things that I need to do in order so that I'm getting good sleep regularly?", because not only will you benefit in the short term, you'll benefit in the long run, and it can change so much about how you're living your life.
- Rhonda: So what do we need to do?
- Dan: Okay. All right. We were talking earlier, so the things that matter are timing, intensity and duration. We talked about duration. Timing is really critical...
- Rhonda: We're talking about light, right? Exposure? Or no, sleep.
- Dan: Sleep duration. With my company, Dan's Plan, we try to help people live as a restorative sleeper. So the aspiration there is, you wake refreshed and you feel alert all day, every day. Cool. I want that. What do I do, right? So then the determinants of good sleep, the things that matter for sleep are timing, intensity and duration. Duration is just getting adequate time for sleep within a 24 hour period. Timing is everything to do with our circadian rhythms, right? So if you usually go to bed at midnight and wake up at eight, but then on one night you go to bed at four and wake up at noon, even though it's eight hours, it's not going to be the same, right? And that's because so much of sleep is based off of a circadian rhythm. So when you're doing memory formation, when memory formation is happening in your brain at night, there is a component of that that is absolutely determined by what time of day your body thinks that it is. So to get very efficient REM sleep, then if you're usually getting great amount of REM sleep at 4 a.m., but if that's now all of a sudden shifted to 8 a.m. because that's just happened to have been when you're getting your REM sleep, it's just not going to be the same. You're not going to be storing memories as well, you're not going to be clearing beta-amyloid as well, you're not going to be doing all the things you want sleep to do.
- Rhonda: How long do those effects last? Can you recuperate from them?
- Dan: You can, but think about, a great way to kind of answer that question is, think about how long it takes when you go from San Francisco to Italy, right? That the body can only adjust its circadian timing by about three hours a day. Excuse me.
- Rhonda: What do you mean by that? Like you have a three hour wiggle room kind of thing?
- Dan: It's not necessarily a wiggle room, but if I think, if my body knows that it's midnight tonight at midnight, but then if I want to adjust my schedule so that I'm on New York's clock, it can take me one day if I do everything right to fully adjust my physiology so that I am adjusted to New York time. But if it's more than that, right, so basically you can adjust your own physiological clock by three hours per day.
- Rhonda: I see. Okay.
- Dan: And no more than that, and that's only under like perfect conditions. So when you are shifting the timing of your sleep back and forth, then yeah, there's going to be a little bit of consequence to that. You're not going to be getting as much benefit as you would otherwise if you were sleeping within the same circadian phase. So the lesson there is, not only worry about getting the right amount of time in bed, but also that you've got very consistent timing of your sleep.
- Rhonda: Consistency. Yeah.
- Dan: For intensity, it's not a directly actionable thing, but physical activity and light exposure are going to affect the intensity of your sleep, which is really important, because we want to get, again, a lot of that slow wave activity, between .6 and 1 Hertz, which is the one that's going to clear the beta-amyloid. We want a lot of slow wave sleep, delta sleep, which is from 1-4 Hertz, that's going to clear away a lot of the adenosine which makes you sleepy. All this stuff is happening during different processes. Then REM sleep, you're doing a lot of what's called synaptic rescaling. That's where memories are getting played over and over again, and it's another component of memory formation and brain health. The idea is, what's that one phase of sleep that's important? No, they're all important. And one way to facilitate is, again, adequate time, good, regular timing, so you're sleeping always in the same phase, and then having enough physical activity during the day and enough appropriate light exposure. So that kind of segues into the last part of "The Enduring Mover," which is to not only kind of know what time you should go to bed...knowing what time you should go to bed solves a lot of problems, because it's both timing and duration, really. But then you also want to maintain smart light rhythms day, evening and night. And so what that means is you want to get about a half an hour of bright sunlight during the day, because that strong light signal is going to help anchor your rhythm, and then you're going to want to get, in the evening, dim environmental lights. Do exactly like Rhonda does, if you can: adjust the light bulbs in your house. I actually wear glasses in the evening that kind of solve a lot.
- Rhonda: We have those.
- Dan: And I've got a nice pair made, so they're not really awful-looking.
- Rhonda: Oh, really? You have to show me.
- Dan: I will, I will. I wish I had them here. And I've been wearing those very consistently. What I tell myself is that, all right, if I start to wear these two hours before bed, that is going to help me perform better tomorrow, because, again, it's helping my circadian rhythm know that it is nighttime when it's nighttime. And you can create something called circadian or virtual darkness, where you can see, so you can be in the room with artificial light and you can look at a television screen, you can look at an e-reader, but because it's filtering a lot of that blue light, that blue light is the really potent signal to those cells in the retina that it's day, and you want to block that.
- Rhonda: Philips Hues makes a good light package where you can have the white, the blue and the orange, and have them turn on the white in the day and the orange at night.
- Dan: It's the future.
- Rhonda: It sounds like getting the bright light earlier in the day is probably the most important, right?
- Dan: Yes, because if you don't get enough adequate light during the day, then your susceptibility to artificial light at night, shifting your rhythms is much greater. So I always call daylight "anchoring." It helps really anchor your circadian rhythm. So if you get outside, take every opportunity that you can. If you work in an office, have lunch outside. If you want to take a break, go for a walk. Get outside. If you can exercise indoor versus outdoor, do it outside. It's funny, because some researchers looked at the difference between exercising indoors and outdoors, and some have shown that the same type of exercise, it's healthier for some reason outside, and it's probably circadian rhythm effects.
- Rhonda: Wow. Probably it's healthier outside if it's during the day.
- Dan: Yeah. Right.
- Rhonda: That's really interesting. Some things people can do if they have trouble sleeping are exactly what you mentioned; the timing, making sure they go to bed at the same time, filtering out the blue light at night and getting enough blue light during the day and filtering it out at night, exercise. Some other things that I've personally been interested in but I think they're a little less likely to be have a very robust effect on sleep, is some stuff coming out of a sleep lab in Oxford, and they've been doing some studies, some clinical trials, on nutrition. So I'll tell you, one of the interesting studies that I've read not too long ago, I do a lot of research on omega-3 and serotonin, and serotonin gets converted into melatonin in the pineal gland, so I know a bit about that. But DHA, DHA is important for one of the enzymes that converts serotonin into melatonin, one of the N-acetyltransferases, I think. But it's been interesting, because there have been associative studies that have looked at omega-3 fatty acids and sleep, and they've shown that there is deficiencies correlated with poor sleep and vice versa, but the courses[SP] are associative, there are millions of other things that could be going on. But there's been a couple of controlled trials out of this sleep lab in Oxford that have shown, in children at least, they're given supplemental DHA from an algal source, like 600 milligrams or something like that a day, which dramatically improved their sleep quality. So I found that was interesting, just because there possibly is a mechanism with the conversion of serotonin into melatonin. I don't think that, like I said, I think the other things that you discussed are paramount, much more important. But there's also this interesting literature with B vitamins, B6 specifically, and magnesium, both affect, again, B6 affects the conversion of tryptophan into serotonin, which then gets converted into melatonin, and magnesium affects the conversion of serotonin into melatonin, and it's a GABA agonist. So I know there's been some associative studies with magnesium, and personally there's been people that have reached out to me and told me that, after drinking a smoothie, my smoothie recipe, which has a lot of magnesium, because it's a lot of dark greens, that they sleep better. So it's totally anecdotal, but I find that interesting. Probably good nutrition, cutting out the crap and eating the good stuff, I think that's also probably playing a role, and we may not know all the mechanisms yet, but I think people will start to tease those out soon.
- Dan: So I am not at all incredulous to the idea that good nutrition helps with sleep, because like sleep and exercise are fundamental parts of a healthy physiology, so is nutrition, obviously. And so, part of the ability of the body to generate good sleep is going to be dependent on the health of its cell that are doing that, that are involved in it, which are going to have these nutritional factors that are part of. So there's not great research, there's not really robust research in nutrition on sleep, and I get asked that question a good amount. It's more like if you have a carbohydrate-rich meal before bed or a fat-rich meal, all those sort of things, does it have an effect. And really, it's very equivocal. You might see a little bit of an effect one time, but then it's gone the next time.
- Rhonda: Yeah, that's a short-term.
- Dan: Yeah, short-term. Right.
- Rhonda: It's like, what about the effects of chronic inflammation?
- Dan: Yes.
- Rhonda: If you're eating processed carbohydrates and sugars all the time and you have chronic inflammation, how does that affect your sleep? It probably does.
- Dan: It probably does. So that's the area that is harder to really evaluate super well, but it's also one that's, of course, just as important as anything else. I think generally having a very sound, nutrient-adequate diet, and adequacy is a term that sounds like, I don't know, maybe not that impressive, but it means you're getting enough of whatever you need. All the parts that are kind of involved, all the constituents that are involved in healthy physiological processing. We need a good diet to help us feel kind of robust enough to exercise, for our body to be able to execute on all the components that are necessary to generate good sleep. All these things are connected.
- Rhonda: To repair the damage that we do when we sleep.
- Dan: Repair the damage. Or create more.
- Rhonda: You're CEO and co-founder of Dan's Plan Health, and that's a health and wellness and technology company where you kind of talk about some of these important factors and help people measure things, which I think is super cool, because you have to be able to measure something to know what's really going on, or if you're improving it.
- Dan: Yeah. As Peter Drucker says, "What gets measured, gets managed." It's funny, because this is the field of quantified self, which is trackers like Apple Watch or Fitbit are just some examples of that, and it's this growing movement where there's a lot of excitement. And I speak on this quite a bit, because we can't put too much faith...these devices help when they help us do the activities that get us results. They're not going to be healthy for us, right? So sometimes people think, "Well, if I could just track everything, then everything would be fine." I'm also not really in that camp, either. I created a behavior model called "The Loop Model to Sustain Health Behaviors," and a part of that model is looking at how trackers can help us be more mindful of how we're living, and can also generate adequate insights to kind of maybe find things in our behavioral patterns that we might not be able to see readily or easily otherwise that can help us kind of shift how we live, right? It's all about creating an effective, in my opinion, an effective daily pattern of living, that is going to then affect your trajectory of what your life looks like, in terms of health, and also what you choose to do. I mean, if you have poor health, it's going to significantly affect your own energy, and it's going to affect the version of you that shows up on a day-by-day basis. So all this really has been motivating to me since I lost my father to cancer, and I was in a position where I thought I could help him, and I couldn't really bridge the gap between what I knew and what he needed to hear in order for him to kind of take some behavioral action. And so that kind of sent me off into this mission to say, "Okay, how do you really bridge that gap?" And Dan's Plan, I'll even announce it here, Dan's Plan will cease to exist, and we're launching Human OS later this fall, which I'm really excited about. And so we're going to have health courses, so that you learn what do you need to know on a subject that's important to your health, and so that you can learn it in a way where you can repeat it eight months later after the course. And then programs that should make it really easy for you to kind of follow through on a day-by-day basis, some tracking that helps keep you mindful of how you're living. I'm very, very excited about what I'm doing and why, and It's totally a passion. I heard somebody say the other day, "From misery to mission," and that was kind of my experience. The sadness of experiencing the loss of a loved one to like okay, this is kind of who I am and what I do.
- Rhonda: Right, and you're going to help a lot of other people out there. It's really awesome, Dan. So where can people learn more about this Human OS and about what you're doing, your research and etc.?
- Dan: Sure. You can go to DansPlan.com right now. If you sign up...everybody that is a member...it's free, you get rolled into Human OS when that launches. My research, you can go to PubMed, and I'm going to be submitting a paper to one Nutrition Journal soon, looking at...so I'll just give you a little quick synopsis. The research study that I just finished was looking at cognitive performance after sleep loss, but it was what we called "ecologically relevant." So instead of one day with no sleep at all, it was just, "How did people perform on their cognitive performance tests if they just got one or two less hours for one night?" And what we found is that there was a significant impairment in attention, or alertness, excuse me. Somebody felt either subjectively sleepy, or they have an objective sleepiness or objective reaction time deficit. And both of those, the feeling of sleepiness or a slower reaction time, changed the way that people ate, and so they were much more likely to choose foods that they rated as low-health. And if you think about that, it could be a marker of a defection from personal standards. If you kind of extrapolate or speculate on what else that might lead to, if you're not getting enough sleep, even if you have a standard or a goal to eat a certain way and make it to the gym and do all these things that are related to your health, sleep loss can give you a serious case of the "F-its," and you're like, "You know what? Eh." It's called effort discounting, where you're much less likely to make an effort toward something you value.
- Rhonda: That's super interesting. Congratulations on that. So it also affected attention, though. That could affect the way you're learning and the way you do a task.
- Dan: Absolutely.
- Rhonda: Wow. That was just one to two hours you said?
- Dan: Yeah.
- Rhonda: In one night?
- Dan: For one night. Yeah. So all other previous researchers looked at either one night of total sleep deprivation, or five nights of four hours of sleep. So those types of studies are testing the capacity of the system, so, "Is there anything there at all?" What we were looking at is more like the sensitivity of the system. What's really exciting about this is, yeah, it's great to know that something is there, but it might not be relevant if that's just not realistic or what it's like in the modern world. But missing an hour or two of sleep loss on any given night is very common, very relevant.
- Rhonda: That's common. Yes.
- Dan: What this study shows is that our eating behaviors change in a significant way with just a little bit of sleep loss.
- Rhonda: Wow.
- Dan: Yeah. I'm excited about it.
- Rhonda: So what about like social media?
- Dan: Oh, yeah. So I tweet on DansPlanHealth, and I have to admit, it's mostly just when I read research papers. It's the most like consumer-friendly Twitter, but...
- Rhonda: But they're interesting. Your Twitter is interesting. I really like those things[SP] you tweet.
- Dan: Thanks. Yeah, there's definitely an audience for it, for now. I comb through articles, and the ones that I take and read, I'll usually tweet out some segments of them or the title, just so that people get some exposure. I tweet a lot about microbiota. I'm fascinated by that subject.
- Rhonda: Right. Totally.
- Dan: A lot about sleep and weight, some about cognition, the occasional Golden State Warriors post, just when they win the championship.
- Rhonda: Oakland last night, it was crazy.
- Dan: I bet.
- Rhonda: It was like honking and hollering and fireworks going off just like all night.
- Dan: You've done really well on very little sleep, then.
- Rhonda: I've actually gotten sleep. He didn't.
- Dan: Oh, you didn't? Okay.
- Rhonda: But thanks again, Dan. This was such a like interesting conversation, and I think that people will really enjoy hearing what you have to say, and how important sleep is, and the simple solutions and lifestyle practices they can do to improve their sleep.
- Dan: Thank you so much. Yeah, I call it the "mundane but meaningful." So it's easy to overlook, but once you're armed with knowledge, you can benefit if you act on it. And before we go, I also want to say that I really admire your work and learn a lot from you, so it's an honor to be on your show. Thanks for having me on.
- Rhonda: Oh, thanks, Dan. Glad we're friends.
- Dan: Yeah. Me, too.
- Rhonda: We'll have conversations in the future, for sure.
- Dan: I hope so.
A purine nucleoside composed of a molecule of adenine attached to a ribose sugar molecule. Plays a role in regulating blood flow to various organs as a vasodilator, and, in its role as a neuromodulator, adenosine is believed to promote sleep and suppress arousal. Adenosine is also involved in energy transfer as ATP and ADP, and signal transduction when in the form of cAMP.
The process by which the body responds to stressors in order to regain homeostasis. This can be carried out by means of alteration in HPA axis hormones, the autonomic nervous system, cytokines, or a number of other systems.
A neurodegenerative disorder characterized by progressive memory loss, spatial disorientation, cognitive dysfunction, and behavioral changes. The pathological hallmarks of Alzheimer's disease include amyloid-beta plaques, tau tangles, and reduced brain glucose uptake. Most cases of Alzheimer's disease do not run in families and are described as "sporadic." The primary risk factor for sporadic Alzheimer's disease is aging, with prevalence roughly doubling every five years after age 65. Roughly one-third of people aged 85 and older have Alzheimer's. The major genetic risk factor for Alzheimer's is a variant in the apolipoprotein E (APOE) gene called APOE4.
A prescription drug used to treat insomnia (also known as Zolpidem). Ambien is in a class of medications called sedative-hypnotics. It promotes the activity of GABA receptors in the brain, which slows brain activity to allow sleep.
An area of the brain located close to the hippocampus, in the frontal portion of the temporal lobe. The amygdala governs our responses to fear, arousal, and emotional stimulation. Poor sleep increases activity within the amygdala.
The physiological process through which new blood vessels form from preexisting vessels. This is a normal and vital process in growth and development, wound healing, and in the formation of granulation tissue. However, it is also a fundamental step in the transition of tumors from a benign state to a malignant one.
A molecule that inhibits oxidative damage to DNA, proteins, and lipids in cells. Oxidative damage plays a role in the aging process, cancer, and neurodegeneration. Many vitamins and plant-based compounds are antioxidants.
The shrinking or wasting away of cells, organs, or tissues that may occur as part of a disease process, trauma, or aging.
The body’s 24-hour cycles of biological, hormonal, and behavioral patterns. Circadian rhythms modulate a wide array of physiological processes, including the body’s production of hormones that regulate sleep, hunger, metabolism, and others, ultimately influencing body weight, performance, and susceptibility to disease. As much as 80 percent of gene expression in mammals is under circadian control, including genes in the brain, liver, and muscle.[1] Consequently, circadian rhythmicity may have profound implications for human healthspan.
- ^ Dkhissi-Benyahya, Ouria; Chang, Max; Mure, Ludovic S; Benegiamo, Giorgia; Panda, Satchidananda; Le, Hiep D., et al. (2018). Diurnal Transcriptome Atlas Of A Primate Across Major Neural And Peripheral Tissues Science 359, 6381.
A gene encoding a transcription factor (CLOCK) that affects both the persistence and period of circadian rhythms. CLOCK functions as an essential activator of downstream elements in the pathway critical to the generation of circadian rhythms. In humans, polymorphisms in the CLOCK gene have been associated with increased insomnia, weight loss difficulty, and recurrence of major depressive episodes in patients with bipolar disorder.
A small membranous protrusion from a neuron's dendrite that typically receives input from a single synapse of an axon.
An omega-3 fatty acid found in the human brain and the meat of fatty fish. DHA plays a key role in the development of eye and nerve tissues, and is essential for normal brain function in humans. DHA may also reduce the risk of Alzheimer’s disease1 and cardiovascular disease, and may be useful in treating certain inflammatory conditions, such as rheumatoid arthritis. Dietary sources of DHA include krill oil and the meat and roe of salmon, flying fish, and pollock. [1] Patrick, Rhonda P. "Role of phosphatidylcholine-DHA in preventing APOE4-associated Alzheimer’s disease." The FASEB Journal (2018): fj-201801412R.
Any of a group of complex proteins or conjugated proteins that are produced by living cells and act as catalyst in specific biochemical reactions.
The ability to store and retrieve specific episodes from personal experiences in the past. Episodic memory involves times, places, feelings, and other contexts. It occurs in the medial temporal lobe of the brain, especially the hippocampus.
Beneficial stress that can be psychological, physical (e.g. exercise), or biochemical (hormesis) in nature.
A gene that has remained essentially unchanged throughout evolution. Conservation of a gene indicates that it is unique and essential and that changes in the gene are likely to be lethal or at least highly maladaptive.
A molecule composed of carboxylic acid with a long hydrocarbon chain that is either saturated or unsaturated. Fatty acids are important components of cell membranes and are key sources of fuel because they yield large quantities of ATP when metabolized. Most cells can use either glucose or fatty acids for this purpose.
A neurotransmitter produced in the brain that blocks impulses between nerve cells. GABA is the major inhibitory neurotransmitter in gray matter.
A hormone produced in the gut that signals hunger. Ghrelin acts on cells in the hypothalamus to stimulate appetite, increase food intake, and promote growth. Ghrelin’s effects are opposed by leptin, the “satiety hormone.” Sleep deprivation increases ghrelin levels and feelings of hunger, which can lead to weight gain and metabolic dysfunction.
One of the most abundant non-essential amino acids in the human body. Glutamine plays key roles in several metabolic functions, including protein and glutathione synthesis, energy production, antioxidant status, and immune function. In addition, it regulates the expression of several genes. Although the body can typically produce all the glutamine it needs, during periods of metabolic stress it must rely on dietary sources of glutamine such as meats, fish, legumes, fruits, and vegetables.
A system that clears the brain of metabolites and other waste. The glymphatic system comprises a vast arrangement of interstitial fluid-filled cavities surrounding the small blood vessels that serve the brain. During sleep, these perivascular structures increase in size by more than 60 percent. This allows a “flushing” operation in which waste products can be eliminated. The glymphatic system also facilitates the distribution of essential nutrients such as glucose, lipids, and amino acids, as well as other substances, such as growth factors and neuromodulators.
Relating to or characterized by pleasure. Hedonism is a school of thought that argues that pleasure and happiness are the primary or most important intrinsic goods and the aim of human life.
A small organ located within the brain's medial temporal lobe. The hippocampus is associated primarily with memory (in particular, the consolidation of short-term memories to long-term memories), learning, and spatial navigation. Amyloid-beta plaque accumulation, tau tangle formation, and subsequent atrophy in the hippocampus are early indicators of Alzheimer’s disease.
A region of the forebrain below the thalamus that coordinates both the autonomic nervous system and the activity of the pituitary, controlling body temperature, thirst, hunger, and other homeostatic systems, and involved in sleep and emotional activity.
A critical element of the body’s immune response. Inflammation occurs when the body is exposed to harmful stimuli, such as pathogens, damaged cells, or irritants. It is a protective response that involves immune cells, cell-signaling proteins, and pro-inflammatory factors. Acute inflammation occurs after minor injuries or infections and is characterized by local redness, swelling, or fever. Chronic inflammation occurs on the cellular level in response to toxins or other stressors and is often “invisible.” It plays a key role in the development of many chronic diseases, including cancer, cardiovascular disease, and diabetes.
A peptide hormone secreted by the beta cells of the pancreatic islets cells. Insulin maintains normal blood glucose levels by facilitating the uptake of glucose into cells; regulating carbohydrate, lipid, and protein metabolism; and promoting cell division and growth. Insulin resistance, a characteristic of type 2 diabetes, is a condition in which normal insulin levels do not produce a biological response, which can lead to high blood glucose levels.
A hormone produced primarily by adipocytes (fat cells) that signals a feeling of satiety, or fullness, after a meal. Leptin acts on cells in the hypothalamus to reduce appetite and subsequent food intake. Leptin’s effects are opposed by ghrelin, the “hunger hormone.” Both acute and chronic sleep deprivation decrease leptin levels.
A hormone that regulates the sleep-wake cycle in mammals. Melatonin is produced in the pineal gland of the brain and is involved in the expression of more than 500 genes. The greatest influence on melatonin secretion is light: Generally, melatonin levels are low during the day and high during the night. Interestingly, melatonin levels are elevated in blind people, potentially contributing to their decreased cancer risk.[1]
- ^ Feychting M; Osterlund B; Ahlbom A (1998). Reduced cancer incidence among the blind. Epidemiology 9, 5.
A cluster of at least three of five of the following medical conditions: abdominal (central) obesity, elevated blood pressure, elevated fasting plasma glucose, high serum triglycerides, and low high-density lipoprotein (HDL) levels. Some studies estimate the prevalence in the USA to be 34 percent of the adult population. Metabolic syndrome is associated with the risk of developing cardiovascular disease and diabetes.
The thousands of biochemical processes that run all of the various cellular processes that produce energy. Since energy generation is so fundamental to all other processes, in some cases the word metabolism may refer more broadly to the sum of all chemical reactions in the cell.
A collective term for the community of commensal, symbiotic, and pathogenic microorganisms that live in a particular environment. The human body has multiple microbiotas, including those of the gut, skin, and urogenital regions.
A condition characterized by an extreme tendency to fall asleep whenever in relaxing surroundings.
A type of glial cell that is involved in the production of myelin, providing support and insulation to axons in the central nervous system. A single oligodendrocyte can extend its processes to 50 axons, wrapping approximately 1 micrometer of myelin sheath around each axon.
A type of polyunsaturated fat that is essential for human health. Omega-3 fatty acids influence cell membrane integrity and affect the function of membrane-bound cellular receptors. They participate in pathways involved in the biosynthesis of hormones that regulate blood clotting, contraction and relaxation of artery walls, and inflammation. They have been shown to help prevent heart disease and stroke, may help control lupus, eczema, and rheumatoid arthritis, and may play protective roles in cancer and other conditions. Omega-3 fatty acids include alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). ALA is found mainly in plant oils such as flaxseed, soybean, and canola oils. DHA and EPA are found in fish and other seafood. The human body can convert some ALA into EPA and then to DHA, but the efficiency of the process varies between individuals.
A small endocrine gland found in the brain of mammals. The pineal gland secretes melatonin, a hormone that regulates the sleep-wake cycle as well as other metabolic processes.
The area of the brain located in the front portion of the frontal lobe, just behind the area commonly known as the forehead. The prefrontal cortex is involved in a variety of higher cognitive functions and behaviors such as executive function and expression of appropriate social behavior.
A sustained-attention, reaction-time task that measures the speed with which subjects respond to a visual stimulus. Research indicates increased sleep debt or sleep deficit correlates with deteriorated alertness, slower problem-solving, and declined psycho-motor skills.
A type of neuron located in the ganglion cell layer of the retina. Ganglion cells receive visual information from photoreceptors via two intermediate neuron types: bipolar cells and retina amacrine cells. A small percentage of ganglion cells contribute little or nothing to vision, but, instead, contain melanopsin and contribute to circadian rhythm and pupillary light reflex (the resizing of the pupil).
A small molecule that functions as both a neurotransmitter and a hormone. Serotonin is produced in the brain and gut and facilitates the bidirectional communication between the two. It regulates many physiological functions, including sleep, appetite, mood, thermoregulation, and others. Many antidepressants are selective serotonin reuptake inhibitors (SSRIs), which work by preventing the reabsorption of serotonin, thereby increasing extracellular levels of the hormone.
A person who works on a schedule outside the traditional 9 AM – 5 PM day. Work can involve evening or night shifts, early morning shifts, and rotating shifts. Many industries rely heavily on shift work, and millions of people work in jobs that require shift schedules.
A substance or activity that induces sleep. Soporifics include drugs, endogenous substances, meditation, and the lowering of lights in a room.
A tiny region located in the hypothalamus responsible for controlling circadian rhythms. The SCN maintains control across the body by synchronizing "slave oscillators," which exhibit their own near-24-hour rhythms and control circadian phenomena in local tissue.
The junction between one neuron and another or a gland or muscle cell. Synapses are critical elements in the transmission of nerve signals. Their formation is necessary for the establishment and maintenance of the brain’s neuronal network and the precision of its circuitry.
Distinctive structures comprised of short, repetitive sequences of DNA located on the ends of chromosomes. Telomeres form a protective “cap” – a sort of disposable buffer that gradually shortens with age – that prevents chromosomes from losing genes or sticking to other chromosomes during cell division. When the telomeres on a cell’s chromosomes get too short, the chromosome reaches a “critical length,” and the cell stops dividing (senescence) or dies (apoptosis). Telomeres are replenished by the enzyme telomerase, a reverse transcriptase.
An essential amino acid. Tryptophan plays key roles in the biosynthesis of proteins and is a precursor to several molecules with physiological significance, including melatonin, niacin, and the neurotransmitter serotonin. Inflammation causes tryptophan to be reallocated from serotonin synthesis to that of kynurenine, which then converts to the neurotoxin quinolinic acid, leading to depression. Dietary sources of tryptophan include most protein-based foods, such as meat, beans, or nuts.
A metabolic disorder characterized by high blood sugar and insulin resistance. Type 2 diabetes is a progressive condition and is typically associated with overweight and low physical activity. Common symptoms include increased thirst, frequent urination, unexplained weight loss, increased hunger, fatigue, and impaired healing. Long-term complications from poorly controlled type 2 diabetes include heart disease, stroke, diabetic retinopathy (and subsequent blindness), kidney failure, and diminished peripheral blood flow which may lead to amputations.
Hear new content from Rhonda on The Aliquot, our member's only podcast

Listen in on our regularly curated interview segments called "Aliquots" released every week on our premium podcast The Aliquot. Aliquots come in two flavors: features and mashups.
- Hours of deep dive on topics like fasting, sauna, child development surfaced from our enormous collection of members-only Q&A episodes.
- Important conversational highlights from our interviews with extra commentary and value. Short but salient.