#38 Dr. Guido Kroemer on Autophagy, Caloric Restriction Mimetics, Fasting & Protein Acetylation
This episode is available in a convenient podcast format.
These episodes make great companion listening for a long drive.
The Omega-3 Supplementation Guide
A blueprint for choosing the right fish oil supplement — filled with specific recommendations, guidelines for interpreting testing data, and dosage protocols.
Guido Kroemer, MD, PhD, is a professor at the Faculty of Medicine of the University of Paris Descartes. He serves in a leadership capacity at multiple research and medical institutes in Paris, including the Medical Research Council (INSERM), the Gustave Roussy Comprehensive Cancer Center, the Cordeliers Research Center, and the Hôpital Européen George Pompidou. He is also an adjunct professor at the Karolinska Institute, Stockholm, Sweden.
Dr. Kroemer is an expert in immunology, cancer biology, aging, and autophagy. He is one of the most cited authors in the field of cell biology and was the most cited cell biologist for the period between 2007 and 2013. He is best known for identifying the key role that permeabilization of mitochondrial membranes plays in programmed cell death.
His work has elucidated the intricate mechanisms involved in mitochondrial cell death control, the molecular pathways associated with cell death inhibition, and the role that cancer cell death plays in inducing immune function. In fact, he demonstrated that the therapeutic success of anticancer chemotherapy is mediated by the immune response against stressed and dying tumor cells. His groundbreaking work has been recognized in numerous awards from organizations in the fields of science, medicine, pharmacology, and cancer research.
Dr. Kroemer completed his medical degree and postdoctoral training at the Collège de France, Nogent-sur-Marne. He completed his doctoral degree in molecular biology from the Autonomous University of Madrid.
Autophagy is a highly conserved adaptive response to stress. During autophagy, a spectacular event in cell biology that is observable under a microscope, the cell gathers unnecessary or dysfunctional cellular components such as protein aggregates, pathogens, or damaged organelles into vesicles and delivers them to lysosomes for destruction, releasing proteins, lipids, carbohydrates, and nucleic acids for energy and re-use. The primary goal of autophagy is the maintenance of homeostasis in the face of changing cellular conditions and stress.
Autophagy activation relies on nutrient sensing
Integral to the mechanisms that regulate autophagy is nutrient sensing. In particular, the cell responds to changes in cellular levels of acetyl CoA, an end product of nutrient metabolism. Acetyl CoA acetylates or deacetylates key proteins involved in autophagy (such as mTOR and AMP kinase), thereby serving as a common regulator for the many pathways that lead to autophagy induction or inhibition.
Alterations in nutrient status that regulate autophagy
Starvation and fasting
In the fed state, the body synthesizes essential cellular components from readily available macromolecules and stockpiles the surplus. In the fasted state, however, cellular reductions in acetyl CoA switch on homeostatic mechanisms that mobilize those stockpiles via autophagy. Although the duration of nutrient deprivation necessary to induce autophagy varies among mammals, when mice or human volunteers experience starvation, autophagy can be observed on the whole-body level.
Prolonged fasting – a period of voluntary starvation that typically exceeds 48 hours – sets off a wide range of metabolic events, including the activation of cellular and systemic cleanup programs such as apoptosis and autophagy. Many people may find the prolonged fast too onerous, but the fasting-mimicking diet, an approach that recapitulates many of the same effects of prolonged fasting with a hyper-low calorie, low protein, higher fat diet stretched out over a longer interval of five days, may offer a more palatable strategy for activating autophagy.
Calorie restriction mimetics
Another strategy for modulating acetyl CoA levels involves intake of caloric restriction mimetics, compounds that “trick” cells into inducing autophagy even in the setting of sufficient nutrient levels. Examples of caloric restriction mimetics include resveratrol and spermidine, two dietary compounds present in red wine and cheese, respectively.
Exercise
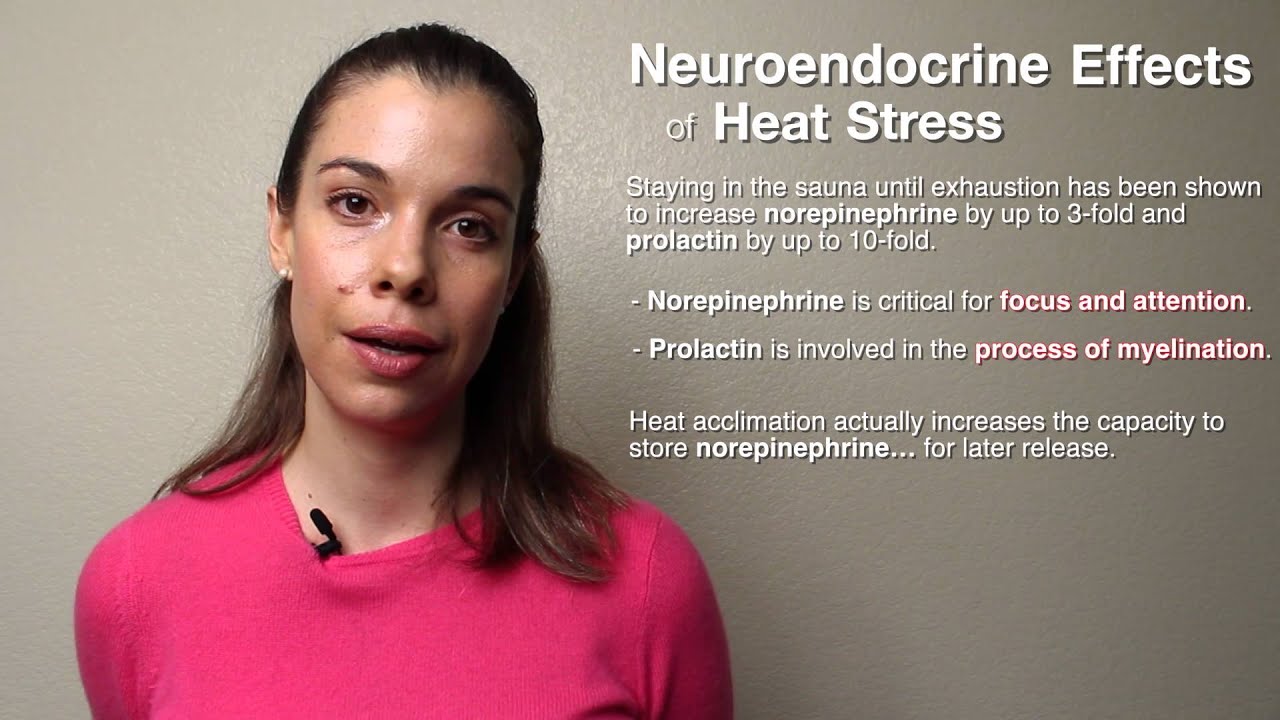
The many health benefits associated with exercise are well known and include extension of lifespan and protection against cardiovascular diseases, diabetes, cancer and neurodegenerative diseases. Some of these benefits may be due to the fact that exercise induces autophagy in the brain and several organs involved in metabolism, including the liver, pancreas, adipose tissue, and muscles.The greatest benefits are observed with endurance training, which induces autophagy in mice, mediating the deleterious effects of diabetes and obesity.
Autophagy and mitochondrial health
Defective and aging mitochondria contribute to metabolic dysfunction and disease. Mitophagy, the selective degradation of dysfunctional mitochondria, helps ensure that the body’s cells are metabolically efficient. These old or defective mitochondria self-identify as dysfunctional, offering themselves for mitophagy, like martyrs on behalf of the cell. Mitophagy ultimately serves as a trigger for mitochondrial biogenesis, the process by which new mitochondria are produced. Failures in mitophagy are associated with several chronic diseases, including cardiovascular disease, kidney disease, and Alzheimer’s disease.
Autophagy and neurological health
Parkinson's disease, a neurodegenerative disorder characterized by mitochondrial dysfunction and energy deficits in dopaminergic neurons in the brain, may be due in part to mitophagy failure. A growing body of evidence suggests that mitophagy is compromised in Parkinson's disease and promotes the accumulation of dysfunctional mitochondria. Impaired mitophagy likely contributes to the aggregation of misfolded proteins, which in turn impairs mitochondrial homeostasis.
Autophagy as a critical trigger for immunosurveillance
Autophagy plays a role in triggering mechanisms of immunosurveillance by facilitating the release of ATP from dying cells, which attract the attention of myeloid cells via a special class of receptor known as purinergic receptors. Activation of this important system of immunosurveillance is a predictor of long-term efficacy of chemotherapy and may help to explain the complex relationship of autophagy with cancer, wherein the initial suppression of autophagy may help prevent attracting undue attention from the immune system, but may later facilitate ongoing transformation. In later stage cancer, autophagy may be reactivated to help cells in their pursuit to continue gaining a foothold in the otherwise hostile tumor microenvironment of the body.
In this episode, Dr. Kroemer describes the complex process of autophagy and how it influences many aspects of health and disease, including cancer, neurodegenerative disease, and aging, and how modulation of autophagy may represent a promising therapeutic approach for extending human lifespan and healthspan.
Learn more about autophagy in this topic article from FMF.
This episode is decidedly focused on autophagy, an important cellular program that is inducible by dietary fasting and has broad implications for aging and cancer. Autophagy discussion includes:
-
- How the 3 main signals that activate autophagy all involve nutrient sensing.
-
- The role of different types of fasting and nutrient deprivation in autophagy.
-
- How different types of exercise can induce autophagy.
-
- How a specific type of autophagy called mitophagy keeps mitochondria healthy.
-
- How autophagy has been shown to slow cellular aging.
-
- How autophagy prevents neurodegenerative diseases by clearing away protein aggregates.
-
- The role of autophagy in cancer as a possible double-edged sword.
-
- How certain compounds known as caloric restriction mimetics (or fasting mimetics) including resveratrol, spermidine, hydroxycitrate can induce autophagy by tricking the cell through the modulation of one or more of the 3 main autophagy signaling pathways.
Learn more about Dr. Guido Kroemer
TL;DR
Fasting Autophagy
Nutrient deprivation → ↑ Protein Deacetylation (↓ cytosolic Acetyl CoA) + ↓ mTOR + ↑ AMP Kinase → Autophagy
Hydroxy Citrate Autophagy
↓ ATP citrate lyase activity → ↓ Protein Acetylation → Autophagy
Spermidine Autophagy
↓ Acetyltransferase activity (especially EP300) → ↓ Protein Acetylation → Autophagy
Resveratrol Autophagy
↑ Detacetylase activity (especially SIRT1) → ↓ Protein Acetylation → Autophagy
... and... more generally...
↑ Protein Deacetylation → Autophagy
The relationship between cancer and autophagy is complex...
↓ tumor suppressor gene activity → ↓ autophagy → survival of pre-malignant cells → ↑ autophagy as a malignant adaptation
-
How genetically inhibiting autophagy actually increases cellular sensitivity to death and how this was counterintuitive because autophagy was thought, at one time, as a type of activity predominantly concerned with actually initiating cell death.
-
The external signals causing autophagy.
-
The role of growth factors in transporting nutrients from the outside world into the intracellular space.
-
Autophagy as a process that destroys bioenergetic macromolecular reserves including proteins, lipids, and nucleic acids to generate energy.
-
How declines in the ATP (energetic) status of the cell trigger autophagy by increasing the activity of a pathway known as AMP Kinase.
-
How reductions in the cytosolic pool of acetyl-CoA as a consequence of reductions in glycolysis, amino acid catabolism, or beta-oxidation, ultimately result in the de-acetylation of hundreds of cellular proteins involved in autophagy. Nutrient deprivation → ↑ Protein Deacetylation (↓ cytosolic Acetyl CoA) + ↓ mTOR + ↑ AMP Kinase → Autophagy
-
The role of the inhibition of mTOR and activation of AMP Kinase in cellular autophagy. mTOR is a pathway robustly activated by IGF-1 and associated with increases in cell growth, proliferation, motility and protein synthesis. AMP Kinase, on the other hand, is a pathway important in regulating cellular energy homeostasis by inhibiting synthesis of fatty acids and triglycerides and activating fatty acid uptake and beta-oxidation in the liver.
-
The indirect relationship between protein acetylation status (and cytosolic acetyl CoA availability) and the suppression of mTOR and activation of AMP Kinase in cellular autophagy.
-
The possibility of using selective nutrient restriction as an autophagy-inducer instead of more generalized nutrient deprivation or fasting.
-
Cytoplasmic protein deacetylation as a potential surrogate marker for fasting-induced autophagy (still undergoing validation) but possibly not other forms of autophagy, such as the kind pharmacologically induced by interaction with a protein involved in vesicle-trafficking processes called Beclin 1.
-
How a protein called LC3 associates with structures called autophagosomes to facilitate autophagy in response to deacetylation it undergoes. Note: this sirt1-mediated deacetylation of LC3 is induced as an important response to cell starvation.
-
The special flow cytometry needed in order to measure some of the proteins associated with the activation of autophagosomes in autophagy.
-
The desirability of being able to know and test whether or not your fasting is triggering robust autophagy or not.
-
The minimum amount of fasting necessary to activate autophagy. (We already know prolonged fasting is a robust activator of autophagy.)
-
Whether or not time-restricted eating or 16:8 intermittent fasting reliably induces autophagy in any of our tissues.
-
The important differences between prolonged fasting in humans and the rodent animal models used in studies.
-
The ~12-hour half-life of IGF-1 and whether or not that has any implications for the potential of autophagy in shorter duration fasts.
-
The effects of long-term caloric restriction on markers of cellular autophagy in humans.
-
The effect of an every-other-day eating pattern in rodents and how this pattern actually mimics the longevity producing effects of caloric restriction but with the advantage of stabilizing long-term at a more normal body weight. (Note: Dr. Kroemer is quick to point out that this type of intermittent fasting is more dramatic than it would be in humans because of differences in metabolism… the animals actually experience a 10% oscillation in body weight from this pattern!)
-
The effect of exercise (especially endurance exercise) on autophagy in muscle tissue.
-
The role of autophagy as a mediator of the anti-obesity and anti-diabetic effects of endurance exercise. Study.
-
The differences between macroautophagy, microautophagy, and chaperone-mediated autophagy.
-
The difference between autophagy that is dictated by demand (nutrient stress) versus autophagy that occurs as the need arises to recycle damaged organelles.
-
How damaged organelles change the composition of their surfaces in order to decorate them with signals for the stimulation of their engulfment by the autophagosome.
-
The many, many names autophagy has when we are talking about it in the context of specific macromolecular structures and organelles (e.g. mitophagy for mitochondria, pexophagy for peroxisomes, reticulophagy for endoplasmic reticulum, ribophagy for ribosomes, and virophagy for viruses).
-
How autophagy from nutrient deprivation still prefers to first recycle organelles that have been slightly marked… in other words, that are already aged or slightly damaged.
-
How mitochondrial use ubiquitination, a process which occurs when these organelles begin to lose their membrane potential, in order to signal damage and to ensure preferential targeting by the autophagic machinery. ↓ mitochondrial transmembrane potential → ↑ ubiquitination → ↑ mitophagy
-
The coordinated manner in which mitophagy and mitochondrial biogenesis act together in a closed feedback loop in order to preserve mitochondrial quality while preserving the total pool of functioning mitochondria. Study.
-
The changes that can occur in total mitochondrial pool as cells adapt to take on new metabolic profiles through a mitophagy-mediated process. This can occur as cells differentiate into new cell types that are specialized for glycolytic energy generation.
-
The role autophagy plays in the prevention of neurodegenerative diseases caused by protein aggregates.
-
How autosomal recessive mutations (where both parents must contribute a defective gene for PD to arise in the offspring) in a kinase protein called PINK1 disrupts its ability to recruit a protein called Parkin that mediates the targeting of mitochondria for mitophagy. ↓ PINK1's kinase activity → ↓ parkin recruitment → ↓ mitophagy → ↑ accumulation of damaged mitochondria
-
Mitochondrial membrane permeabilization as a death signal due to the release of dangerous proteins contained in the mitochondria.
-
-
The evolutionarily-conserved sickness response (food avoidance) as a way of beneficially altering immune responses through altered metabolism and autophagy.
-
The surprising increase in lethality that happens when mice are force fed (glucose in this case) while exhibiting sickness response from a bacterial challenge. Study.
-
The effects of an anti-malarial known as chloroquine which has some cytotoxic effects in cancer cells, but is actually (surprisingly) an inhibitor of autophagy.
-
Studies of the lysosomal disrupter and anti-malarial chloroquine in combination with chemotherapy in the treatment of cancer.
-
The differential roles autophagy plays in the progression of cancer in pre-malignant cells, when it is suppressed, versus in malignant cells, when it is sometimes used as an adaptation helpful to the survival of malignant cells experiencing environmental stress. ↓ tumor suppressor gene activity → ↓ autophagy → survival of pre-malignant cells → ↑ autophagy as a malignant adaptation
-
How inhibition of autophagy by itself is sufficient to induce oncogenesis, particularly in leukemia.
-
How cells undergoing autophagy can release ATP into the extracellular space where it can function as a signal that recruits and activates immune cells against tumor antigens through the activities of purinergic receptors. ↑ autophagy → ↑ extracellular ATP → activation of purinergic receptor-mediated immunosurveillance
-
The importance of the triggering of this immunosurveilance system as part of the cell death associated with chemotherapy.
-
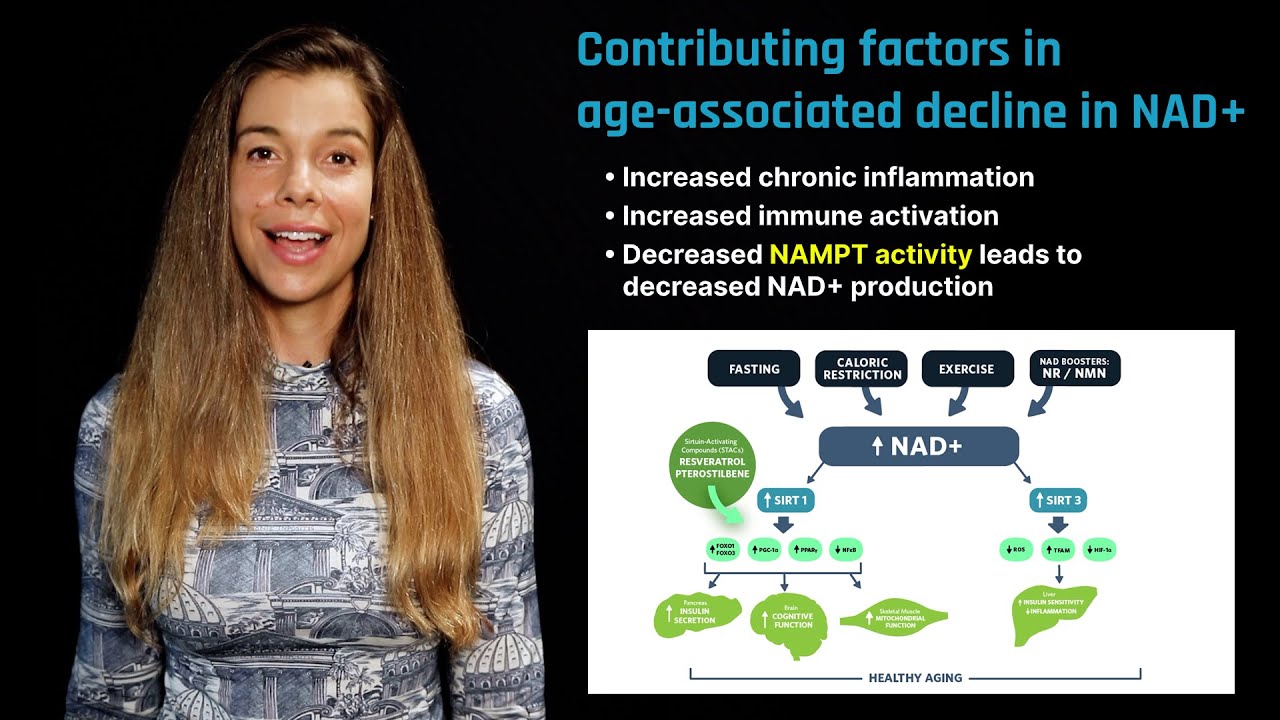
The class of compounds known as “caloric restriction mimetics” that affect autophagy by perturbing various pathways in such a way as to reductions in cytosolic acetyl CoA and protein deacetylation in a manner similar to nutrient deprivation. Examples include: hydroxycitrate (inhibits ATP citrate lyase), spermidine (inhibits Ep300, a protein acetyltransferase), and resveratrol (activates deacetylases).
-
How intestinal bacteria may produce as much as 1/3rd of the body’s spermidine and how this production rate can be manipulated by probiotic and dietary interventions.
-
How the ability of caloric restriction mimetics (CRMs) to induce a type of autophagy that provokes immunosurveillance potentially offers an opportunity for synergy when used in combination with chemotherapeutic agents in the treatment of cancer. Study.
-
How the inhibition of autophagy in malignant cells or destruction of the extracellular ATP released by cells undergoing autophagy is able to abolish the favorable interaction between caloric restriction mimetic drugs and chemotherapy.
-
The tendency for dietary consumption of caloric restriction mimetics, particularly hydroxy citrate, to induce autophagy and reduce weight gain in mice fed an obesogenic diet. Study.
-
Dr. Kroemer’s personal intermittent and prolonged fasting practices and his habit of consuming foods that may contain some natural quantities of caloric restriction mimicking compounds.
-
The autophagy-enhancing effect of coffee (with and without caffeine).
- Rhonda: Hello, everyone. Today I'm sitting here with Dr. Guido Kroemer, who is a professor at the University of Paris Descartes. He is a cell biologist who has made major contributions to understanding the role mitochondria play in cell death. He has also published numerous publications in the fields of cell biology, cancer biology, immunology, aging, and autophagy. The latter of which, I suspect, we're probably going to talk a lot about today because it's such an important topic.
- Dr. Kroemer: So, autophagy is a spectacular phenomenon in cell biology, one that you can see with your eyes because cells become vacuolated when this process is induced. So you can see it by light microscopy and better, of course, by electron microscopy. It is a process that consists in sequestering portions of the cytoplasm of the cell and then digesting them to recycle the material and to degrade macromolecules into micromolecules, metabolites, and to allow rebuilding the structures that have been destroyed. So technically, it works in the sense that the mouth that is involved in this self-digestion process is the autophagosome. So, it will sequester portions of the cell in the cytoplasm. It can be entire organelles including mitochondria, it can be protein aggregates, it can be bacteria or viruses that invade the cell, and this autophagosome, once it closes, will fuse with the lysosomes, which is the sort of stomach of the cell. And in the lysosome, that has been fusing with the autophagosome, which is then called Autophagolysosome, the luminal content will then be digested.
- Rhonda: So you mentioned the digesting of these multiple organelles or mitochondria, but also protein aggregates, and viruses, bacteria, pieces of chromatin, and things all seem to be sort of things that at least in the sense, if you're looking at the aggregates, and you know, damage that occurs in a cell, seems to be something that's associated with aging in general. So it's sort of like, kind of seems like it's getting rid of all these damaging, potentially damaging, not just aging but also obviously, an infection. But this process is getting rid of these damaging, potentially damaging molecules and aggregates and mitochondria which are defective. What is the actual goal of autophagy is? Like you said, is to get rid of these defective things to then provide energy?
- Dr. Kroemer: Well, it's actually interesting to look at the history of autophagy. The name comes from "autos phagy" in Greek which means "self-eating." And it's actually a linguistic invitation to think about self-mutilation and self-destruction and cell death. And actually, the phenomenon is observed mostly in the context of stress. So cells, when they are stressed, will often undergo an autophagic reaction which occurs before the cells die. And so, this chronology of the phenomenon has been also an invitation to think that autophagy is a mechanism that leads to cell death until it has been understood that inhibition of autophagy, which can only be achieved in a specific way by genetic tricks, will actually sensitize cells to cell death induction. And so, this means that autophagy is a means of adaptation to stress and a technique of the cell to avoid cell death. So, the primary goal of autophagy is adaptation to changing conditions and adaptation to external stress, and at the end, avoidance of the unwarranted demise of the cell.
- Rhonda: You bring up so many important points that I'd love to touch on. The first is the external signals that are actually causing autophagy. You mentioned it's a response, it's a generalized response to stress. Like, you know, mostly probably a hormetic type of stress, but even...this is another question I'll have for you later, the differentiating between the type of stress that can cause autophagy versus actually pushing it over to cell death. But in terms of the actual external signals that...the main ones that we know about that cause autophagy, a lot of them have to do with nutrient sensing.
- Dr. Kroemer: Exactly. So, perhaps the most physiological way, to induce autophagy that is phylogenetically conserved from yeast to primitive animals to ourselves is nutrient deprivation, starvation, hunger. And so, the idea is that a cell that is deprived from its energetic supply, which can be the absence of nutrients or the absence of growth factors that are required for these nutrients to be transported from the outside world into the intercellular space or the absence of oxygen, all these factors can induce autophagy, and the cells actually will destroy its bioenergetic reserves, which are macromolecules, proteins, lipids, and ribonucleic acids to generate energy.
- Rhonda: In terms of the energy part, I was reading about like three really major pathways that seem to lead to autophagy. One, being the actual energetic charge of the cell, like ATP status. When that lowers, that activates the AMP Kinase pathway. And then the amino acid sensing pathway, which then when you don't have enough amino acids, that can basically inhibit mTOR. And then there's a third one, the protein assimilation pathway, which I'm not as familiar with essentially how that activates autophagy.
- Dr. Kroemer: So, it's actually extremely easy. When you think about basic biochemistry, one of the central metabolites is acetyl-CoA. And so, the cytosolic pool of acetyl-CoA determines the level of protein acetylation for the simple reason that acetyltransferases, which you see acetyl, moiety of Acetyl-CoA, to transfer it on lysine residues in proteins. Acetyltransferases are having a low affinity for Acetyl-CoA as compared to kinases which have a high affinity for ATP. So if you vary the ATP concentration in the cell, it has little impact on phosphorylation reactions. But if you vary acetyl concentrations, it has a major impact on the acetylation level of cellular proteins. So that's a major difference. And so, since acetyl-CoA is built in the degradation of glucose, a glycolytic pathway, from pyruvate or in the catabolism of branched amino acids, as well as a final product of beta-oxidation. All major nutrients are actually supplying Acetyl-CoA as an end product. And taking away glucose or amino acids or fatty acids will cause a reduction in the acetyl-CoA pool which is important to note, it is a cytosolic acid cetyl-Co-A pool that is accounting for autophagy regulation. And this reduction of acetyl-CoA in the cytosol will cause deacetylation at the end of cellular proteins, hundreds of different proteins, and hence, a sort of multi-pronged induction of major subpathways of the apoptotic process. Autophagy is actually a very complicated process that involves dozens, perhaps hundreds, of different proteins and is regulated by hundreds, perhaps thousands, of additional proteins. And so, this common regulation by acetylation is very efficient in stimulating the autophagic pathway. As a side effect of deacetylation reactions, you usually also observe from the inhibition of mTOR and the activation of AMP Kinase. So, everything comes together at the end. There's no exclusivity for one or the other pathway. They are connected.
- Rhonda: Really? So, changing the acetylation status of proteins affects mTOR and AMP Kinase?
- Dr. Kroemer: Yes. Indirectly, we don't know how this actually works in molecular details.
- Rhonda: Because that was sort of, my next question was I know that if you take cultured cells in a dish and you just...you're doing some, you know, specific nutrient withdraw, you withdraw amino acids when you withdraw glucose, or you withdraw glutamine, you can induce autophagy. But in the whole organism, for example, in mice and in humans, ultimately, you know, can you just limit your protein intake for a week and induce autophagy even in the presence of a normally caloric diet where you're still getting enough energy.
- Dr. Kroemer: That's a good question. We have never tested to selective completion of one or the other nutrient, I suppose that this would work, because protein depletion may affect a newer endocrine factors like insulin growth factor that, at the end, will, due to its depletion, decrease the transport of glucose into the cells. And hence, stimulate autophagy. But it has not been tested thoroughly in mice. What we usually do is we starve mice and sometimes human volunteers completely from any kind of caloric uptake, and in this case, we do see, at the whole body level, that in all major cell types, perhaps with the exception of the brain that is somehow buffered against this effect, protein deacetylation occurs mostly in the cytoplasm.
- Rhonda: And that's a biomarker of autophagy, you would say?
- Dr. Kroemer: Well, it's too early to say that it is a surrogate or proxy of autophagy. So far, we have not been able to dissociate the two phenomenon, autophagy and protein deacetylation, in the response to nutrients. However, when you induce autophagy by pharmacological tricks, such as cell permeable peptides that dissociates an inhibitory interaction between a Golgi protein and Beclin 1. You can induce autophagy without that protein, deacetylation would occur before. And similarly, when you give chemical inhibitors of mTOR like rapamycin or the rapalogs, there's also no protein deacetylation. So, you can induce autophagy without protein deacetylation which means that the proxy would be imperfect. So we do have a system to measure autophagy which is relatively easy to be used in experimental systems which is the study of the redistribution of LC3 and other members of the same family that are usually diffusely distributed all over the cell, mostly in the cytosol, and then we'll aggregate or redistribute towards autophagosomes and autolysosomes. So they acquire a punctate distribution small dots in the cytoplasm and these dots can be seen by fluorescence microscopy if LC3 is labeled by immunofluorescence or when it is fused with green fluorescent protein or similar biosensors. And so, in humans, the only accessible cell type is the circulating white blood cell, the leucocyte. So we can draw blood and determine by immunofluorescence the redistribution of LC3 from a diffuse to a punctate from a pattern. And this is then a sort of detection of autophagy that can be applied to human beings as well.
- Rhonda: That seems like it's kind of complicated though for your standard clinic to be able to use immunofluorescence to look at some leukocytes, circulating leukocytes, right? I mean that's more...
- Dr. Kroemer: Well, you need some technology. Especially, ordinary cytofluorometry cannot be used for this kind of approach, because the standard cytofluorometer just measures an intensity of fluorescence signal per cell not its subcellular distribution. So there are cytofluorometers that take pictures of the cells that are flying in front of the detector, and using these pictures and analyzing them by image analysis software, allows them to quantitate the redistribution of LC3 to autophagosomes.
- Rhonda: So there is hope for a non-invasive clinically relevant biomarker for autophagy but there still, it seems like there needs to be more work done before that actually happen...before I can go to my doctor and say, "I did a four-day fast. I'd like to see if I've activated autophagy. Can you please draw some blood." Right? We're not quite there yet.
- Dr. Kroemer: Yeah, it would be wonderful to have the reward of measuring autophagy as a result of fasting and to get an objective incentive as a biomarker for doing that.
- Rhonda: Right. So it kind of brings up another question I had which related to when you started talking about how you can fast, and fasting in organisms like rodents and also in some human volunteers does induce autophagy. And the question that I had for you is, like, I've talked with Dr. Valter Longo, he was on the podcast, and he talked quite a bit about his research on prolonged fasting in both rodents and also in humans and how the prolonged fast, at least, in rodents is 48 hours, which in humans is around 4 days, 4 to 5 days. And that was able to very robustly, not only activate autophagy, but also cell death, and that was followed by a regeneration period. But, the question is do we know what the minimum amount of fasting time is for humans or rodents that can activate autophagy? So for example, when I'm not pregnant, I usually followed a very time restricted eating schedule where I like to eat all of my food within at least 10 hours, and then I fast for 14 hours every night. Some people do even more strict. They eat within 8 hours and they fast for 16 hours. Does that 16-hour fast induce any autophagy in any of our tissues? Is there any evidence, do we know?
- Dr. Kroemer: We don't know. So, Craig Thompson published a paper on circadian variations in hepatic autophagy. So you know that mice don't eat during the day and they eat during the night, and so, the entire cycle is inversed. And he observed that as a result of not eating during the day, there was more autophagy in the liver. So this result is intriguing. It has not been, to my knowledge, extrapolated to other organs. And it still certainly requires more profound studies.
- Rhonda: Okay. When you say during...
- Dr. Kroemer: So what we did on circulating leukocytes is that we needed to wait for three or four days to see a massive induction of autophagy. There's a fundamental difference between rodents and humans, and so, the two days that you have been alluding to cause a 20% weight loss in mice, that are, at this time point, at the verge of death. Another day would potentially kill them. And so, 20% is a lot, so imagine this for yourself.
- Rhonda: In two days.
- Dr. Kroemer: In four days, a human being only loses one to two percent of his or her weight.
- Rhonda: Is that because they have a higher metabolism, rodents do, or...?
- Dr. Kroemer: Yeah, it's certainly linked to the change in the surface volume ratio that is classically associated with an accelerated metabolism.
- Rhonda: Yeah, okay. That sort of... So we don't really know to what extent autophagy can be occurring in a shorter intermittent fast. There's some hope that it does. I mean, I know, for example, you mentioned IGF-1 and how IGF-1...lowering IGF-1 is important for inducing autophagy because in the whole mTOR pathway and so on. But I do know that the half-life of IGF-1 is, in a serum at least, is around 12 hours. So, the question becomes well, okay, if you start to lower IGF-1, after 12 hours, is do you still need more to occur, like more ATP depletion, more...what...you know, what is it that needs to happen to actually send a signal to the cells to go, "Oh, I'm stressed. I need to start eating my whatever organelle or damaged proteins or something." So is that something that people are currently investigating? Like, the minimum amount of time that it would sort of take to induce, for fasting at least, to induce autophagy.
- Dr. Kroemer: It's an extremely interesting question that is easy to be answered in rodents, and difficult in humans. Because it may be easy to find a volunteer who fasts and allows for regular blood drawing, but it will be very difficult to find a volunteer who fasts and allows for liver, muscle, or skin biopsies.
- Rhonda: Right, right. It kind of reminds me there was a study I was actually reading the other day that was done in the Caloric Restricted Society. You know, there's a group of people that are out there practicing caloric restriction which typically is eating around, what, 30% less food than you normally would eat or something like that. A lot more difficult for people to maintain, I think, than intermittent fasting is, but there was a study that was published. And these individuals had been doing caloric restriction for about six years, plus or minus. I'm sure you've seen the study. But they did muscle biopsies on them and they measured LC3. They measured some of the biomarkers of autophagy, I think Beclin and some other things. And then they measured heat shock proteins, which are also a stress response. And it was, you know, like in some cases, the heat shock protein, HSP70, was elevated by 12 fold compared to age-matched, lean controls that eat more of a Western-type diet. But you know, the fact of the matter is that they did do a muscle biopsy. Autophagy was activated. You know, the stress response pathway, in general, was activated. But six years of doing caloric restriction is not very sustainable for the majority of the population in the, you know, at least in the United States and in Western world.
- Dr. Kroemer: Actually, in mice, you can obtain exactly the same longevity extension that you would obtain, the 30% of caloric restriction by intermittent fasting. So, it's logistically much more difficult. Imagine, you have to weigh, for each mouse, the amount of food that they would eat normally, subtract 30%, put it in the cage, individual cages because calorically restricted mice tend to eat each other.
- Rhonda: Oh, wow.
- Dr. Kroemer: Yeah, they become aggressive because they are hungry.
- Rhonda: They become cannibals.
- Dr. Kroemer: Yeah, they become cannibals. So, it is logistically much more simple to take out the food from the cage completely, and to put back the food on the next day. So it's one day without any food, and another day with normal nutrition. And at the end, so, you have an oscillation of the weight of the mice, 10% every day. These oscillations tend to become smaller because the mice somehow adapt to this sort of stress, but the final result is that the intermittently fasted mouse has the same weight as a normally fat mouse. A difference with the calorically restricted mouse, it weighs also 20% to 30% less. And in spite of this difference in the body weight, intermittent fasting allows for a lifetime expansion in the same way as does caloric restriction. So, one can also consider that this may be more amusing to have, if I was a mouse, I would probably prefer the intermittent regimen, because it means satisfaction during one day and dissatisfaction on the other day, but not permanent dissatisfaction.
- Rhonda: Most people prefer doing intermittent fasting. I mean, it'll be very interesting to see more studies come out on, you know, the translation of this to humans and, as you mentioned, you needed three days of...was it a water fast they did? Was it a complete fast or they had coffee or...?
- Dr. Kroemer: Coffee. Tea.
- Rhonda: Okay. No food.
- Dr. Kroemer: No sugar, no milk. And water.
- Rhonda: Okay. So three days was enough to, at least, show signs of autophagy in circulating leukocytes. And Valter's work has shown, you know, four to five days and he's done. You know, he's got his fasting and then he's got the fasting-mimicking diet into... Some also hints that that also is enough. So, that's sort of encouraging. It would be more encouraging to have like a 24-hour fast or 48-hour. I mean, that's so much easier to do in general. But the other thing that induces autophagy, you're mentioning the stress response and oxidative oxygen, and it sort of reminded me of exercise and how exercise also induces autophagy. I've seen some studies where in humans, they've looked at muscle, skeletal muscle, and how aerobic exercise and eccentric and concentric exercise all can activate autophagy in skeletal muscle. Do you know if it activates autophagy in multiple tissues? Exercise?
- Dr. Kroemer: That's something that we have not studied. So, it is known that endurance training is particularly efficient in mice to induce autophagy and that it mediates anti-obesity and anti-diabetic effects that are depending, in a way, on autophagy induction, because genetic modifications of the process that leads to autophagy induction, its inhibition, specifically by exercise, can prevent these anti-diabetic effects.
- Rhonda: Really?
- Dr. Kroemer: Yeah.
- Rhonda: Oh, I didn't know that the role of the exercise in preventing diabetes was shown to be dependent on autophagy to some degree. That's very interesting. So, do you think that has to do with the liver, and the like pancreas, somewhere... I mean, is it known?
- Dr. Kroemer: To know this in detail, it would be necessary to inhibit autophagy specifically in different tissues and, to my knowledge, this has not been done yet.
- Rhonda: Okay. So do you think fasting while you're like exercising in a fasted state... Now, that's another thing that's...do you think that would be important? Or do we... I mean, I've seen some studies in mice where they claim it is, but mice have a very high metabolism. And so, there's a synergy there. But when you look in humans, it's not so important. Like, the exercise can still induce autophagy in skeletal muscle in humans even without being in a fasted state, but the question is like will you synergize more and...
- Dr. Kroemer: You can speculate, but we don't know.
- Rhonda: I'm giving you a lot of ideas here. So maybe we can kind of talk, shift a little bit into the general role that autophagy plays in some of these age-related diseases, like neurodegenerative disease, cardiovascular disease, and cancer. Talk a little bit about the microautophagy, or is that what you call it, like, when you're talking about the specific degradation of organelles like mitochondria or protein aggregates?
- Dr. Kroemer: So normally, when we refer to autophagy, we talk about macroautophagy, which is the phenomenon that you can see easily by microscopy. Because of the formation of the autophagosomes that are big enough to be seen by conventional microscopy, face contrast, and especially of course when you enhance a solution by immunofluorescence or similar technologies. So, there are other types of autophagy that are less well studied. Like, chaperone-mediated autophagy or microautophagy where basically proteins or portions of the cytosol are introduced directly into lysosomes. So you don't need the mouth of the process or autophagosome, you just need the lysosome. And they are much less studied. And then there's a special case among different kinds of macroautophagy. So to be very simple in the dichotomy, there is the case that autophagy is dictated by general stress or general absence of nutrients, which means that it is dictated by demand. So the cell needs to eat some portions of itself to adapt to nutrient stress, and the other kind of autophagy is dictated by the offers. So a damaged organelle will change the composition of its surface in a way that it is decorated by signals for stimulating its engulfment by the autophagosome. And so, it's another kind of autophagy that then can be specific. Specific for organelles of different types like mitochondria, and it is called mitophagy, or for peroxisomes, and it is called pexophagy, for the endoplasmic reticulum, and it's called reticulophagy, specific for ribosomes, ribophagy. Perfect, yes. And specific for viruses, and it is called virophagy. And the two processes may also interact in a way. So when you stimulate general autophagy by activating the nutrient sensors, AMP kinase, inhibition of mTOR, or by provoking deacetylation, then you increase the demand, and the autophagy machinery actually prefers in a way to sequester and to destroy those organelles that are already slightly marked for destruction. The protein aggregates that are not yet harmful enough to emit a signal per se but they are there. And so it's a sort of preferential cleaning of the slightly damaged and slightly aging portions of the cell. And this may actually explain why stimulation of autophagy in cells, when they are monocellular organisms or at the organismal level at different organs, can be a sort of device against aging.
- Rhonda: Wow, that was very beautiful explanation. It actually answered a question I was going to ask you which was, you know, the difference between the signal, for example, nutrient generalized autophagy, when you have the nutrient sensing stress that even that can, to some degree, selectively degrade mitochondria, for example, but the actual signal that really does activate mitophagy...when you're talking about mitophagy, it's a little different, right? It's the actual mitochondrial damage, the membrane potential...
- Dr. Kroemer: Yes.so when a mitochondrion is suboptimal in its function, it will decrease its mitochondrial transmembrane potential. And this is a signal to activate enzymes on the surface of the mitochondria that cause ubiquity relation, recruitment of autophagy adapters, and leads at the end to autophagy because of the organelles or the organelle in a way offers itself, it proclaims its sacrifice by autophagy. And so, of course, this is not an all-or-nothing phenomenon. So mitochondria can be aging in the cell, and as they age, they gradually decrease the performance and the mitochondrial transmembrane potential. So, those mitochondria that are most dysfunctional, they will be eaten first if you increase the demand for autophagy.
- Rhonda: That is very cool. And if you are selectively degrading these damaged mitochondria, which are you know, or aged which are damaged, do they get replaced by new mitochondria? Is that a signal for mitochondrial biogenesis?
- Dr. Kroemer: Yes. So in C.elegans, this was a study that actually the whole turnover of mitochondria is regulated. So, there's a sort of coupling between mitophagy and mitochondrial biogenesis.
- Rhonda: That's good to know.
- Dr. Kroemer: So it's very clever, how the system has been designed.
- Rhonda: It's great. So it's not like you're losing...you're not losing the pool of mitochondria. You're effectively losing the defective pool, and you're almost making younger mitochondria. If you're going to make a new mitochondria, then it's going to be young and fresh and not damaged. So it's very elegant way to sort of replenish your mitochondrial population, it seems.
- Dr. Kroemer: So we have to make the difference between homeostatic conditions and, for instance, cellular differentiation when cells change their metabolic program. So the easiest example is yeast that you suddenly place in the glucose-containing medium to allow for the fermentation of glucose in wine or beer production. So these yeast cells don't eat much oxidative phosphorylation, and they essentially rely during the process on glycolysis. So they adapt to this change by destroying most of their mitochondria, by mitophagy. And this makes actually a metabolic adaptation of the yeast cell efficient. Do you have similar examples in the embryonic development of the retina for retinal ganglion cells or the differentiation of macrophages from so-called M0 to M1 macrophages, in which the cells change from oxidative phosphorylation respiration to an essentially glycolytic metabolism that is coupled to mitophagy. And so, inhibition of mitophagy actually avoids the differentiation process in both examples that I just gave to you.
- Rhonda: That's really interesting. So obviously, these processes are not just as a stress response, they're part of development as well.
- Dr. Kroemer: They can be used in multiple different instances.
- Rhonda: Very interesting. And in the case of mitophagy here, it's also it plays an important role in the prevention of neurodegenerative diseases. Correct?
- Dr. Kroemer: Yes. So, most known neurodegenerative diseases are either caused by the aggregation of poorly built protein cell that somehow create protein aggregates that are toxic for the cell. Or they can also be caused by septal deficiencies in the autophagic and lysosomal machineries that lead to the accumulation of unfolded proteins at the end. And so, either the excessive production of unfolded proteins or their reduced removal causes to a slow accumulation of these toxic protein aggregates. Remember that neurodegenerative diseases are slow processes in most cases that manifests with old age. And so, one strategy to treat neurodegeneration, at least theoretically, is to increase autophagic turnover. And so, one technique is actually then to stimulate general autophagy by increasing the demand, by starvation, or by biochemical trickster that substitute for starvation, and to reduce the protein aggregates that are the cause of the disease.
- Rhonda: So these protein aggregates like amyloid beta plaques in Alzheimer's disease or alpha-synuclein in Parkinson's disease. So, basically, the clearing out of those protein aggregates obviously would play an important role not only in prevention but presumably also, to some degree, in help with the treatment. Of course, that's you know, an speculation, but... And then the mitochondria, the one I was thinking about with mitophagy, was the role, at least some of the proteins that are involved in that, like, the PINK/Parkin, and how they seem to be important for Parkinson's disease. Is that accurate?
- Dr. Kroemer: Yeah. So the PINK/Parkin pathway is one pathway among others, that allows for marking mitochondria that are damaged for destruction. And so, inhibition of this pathway leads to the accumulation of malfunctioning mitochondria with major consequences for the cell that harbours cells' mitochondria because all of a sudden bioenergetic metabolism becomes inefficient, reactive oxygen species are produced, and as you know, mitochondria are latent bombs in the sense that they enclose potentially dangerous proteins that once released will activate the apoptotic machinery and cause cellular suicide.
- Rhonda: Yeah. So, that's the question. Do we know the threshold for the stress threshold for, you know, activating autophagy, and when that pushes the mitochondria then to permeabilize and cause cell death? Like, where, for example, with Valter's work in mice, he had done 48-hour fasts and there was both autophagy and massive apoptosis occurring. So, is it just the intensity of the signal that can then say, "Okay, autophagy is not going to work here. We got to die." Or do we know?
- Dr. Kroemer: Well, autophagy in used in most cell types, while apoptosis is occurring in selected cell types. So what Valter has been observing, if I remember well, is destruction of leukocytes, right, white blood cells, which are very easily to be rebuilt. And so, the loss of 50% or 75% of leukocytes can be easily repaired in a few days. And it is a way to adapt the repertoire of immune cells to changing circumstances. It is a way also to inhibit unwarranted inflammatory reactions. So depending on the context, induction of autophagy can be actually a subtle way to avoid excessive inflammation. One example is the so-called sickness response. So, a cat or a dog or a human being or a mouse that is sick, that has a bacterial infection, will hide away, avoid light and noise, and will not eat. It's a classical phylogenetically conserved reaction in most cases of bacterial infection. And so this phenomenon leads to changes in the metabolism. Ketone in the production of ketone bodies, the reduction of glucose levels, presumably also induction of autophagy, and altogether these mechanisms avoid excessive inflammation that may be lethal. So Aslan Medzhitov published a paper in cell last year showing that force-feeding mice or just increasing the glucose levels to a normal concentration was sufficient to make bacterial infection that otherwise would have been able to cope with lethal.
- Rhonda: Wow. So, I know in humans too. And we have a bacterial infection, for example, a stomach virus or something that's bacterial of origin, you don't eat as well. So, it sounds like it's sort of a protective mechanism.
- Dr. Kroemer: It is.
- Rhonda: That's really interesting. I didn't know that. It's very interesting. I want to kind of move on to cancer, just for time purposes. So cancer is another sort of very, it's been, in regards to autophagy, something that I've always sort of been unsure about, because it's very clear to me that preventing the accumulation of damage, you know, pieces of nucleic acid and pieces of chromatin and all sorts of things that can cause inflammation by having damaged proteins around and things like that. Obviously, clearing those out would be very important for preventing cancer. But when it comes to treating cancer, it's not as clear. There seems to be... I mean, for example, you know, there's a very classic drug out there, chloroquine, right, that inhibits autophagy that's used to kill cancer cells. But...
- Dr. Kroemer: Well, it's not exactly [inaudible] or chloroquine is a lysosomal inhibitor. It's a molecule that, due to its charge, will specifically enrich in the membranes of lysosomes, and then causes lysosomal membrane damage, potentially also inhibition of autophagy. But it fundamentally also liberates the potentially toxic content of lysosomes into the cytosolic space.and so, there are a few reports around showing that inhibition of autophagy is not the sole mechanism by which chloroquine can mediate such a toxic effects.
- Rhonda: Okay. Well, that's good to know.
- Dr. Kroemer: The other thing that is important to notice is that chloroquine and hydroxychloroquine, which are antimalarial agents that have been used for a long period, and also actually used for the treatment of rheumatoid arthritis because they have anti-inflammatory properties. Only introduced into clinical trials, most in combination with chemotherapy or radiotherapy to treat cancer. And those clinical trials, so far, are not convincing.
- Rhonda: Okay. So what about the fact that some cancer cells do activate autophagy?
- Dr. Kroemer: So one relatively general mechanism may be that early during oncogenesis, the deletion of tumor suppressor genes or the activation of oncogenes leads to autophagy suppression. So there are several examples for this. And it is part of the process that leads to cellular transformation, because autophagy is a homeostatic mechanism that, if inhibited, favors genomic instability and malignant transformation of the cells. So there are examples on the literature also that dived inhibition of autophagy is sufficient to cause oncogenesis, in particular, in the context of leukemia. And so, later on, when the cells strive and adapt to an ever more hostile microenvironment, hostile because there's too little vascularization for the expanding cancer cells, so initially there are hypoxic areas, there's no normal tissue architecture, so the cells are usually undernourished. The doctor may apply some chemotherapeutic agent which is an additional stress. So there are internal and external stress pathways that the cell has to cope with. And it is an advantage for the cancer cells to reactivate the autophagic process. And so, it has been proposed that inhibition of autophagy would be a way to make the cancer cells more fragile and vulnerable to therapeutic intervention by chemotherapy, radiotherapy, targeted therapies. The problem is that nothing is simple in oncology and that cancer is not just a cell-autonomous disease. It is more. It is not just that one cell has become wild term and has been accumulating genetic and epigenetic changes that make it selfish. No, a cancer cell will only survive if it escapes from immuno-surveillance. So the immune system, fortunately for us, is usually very efficient in eliminating aberrant cells, premalignant cells, and the initial cancer cells. And actually, the inhibition of autophagy that occurs during early oncogenesis maybe also a way for the cancer cells to hide from the immune system. And so, it is complex. It's immunology, multiple different players come into action. Autophagy, for instance, is required for stressed cells to release ATP into the microenvironment. You know, of course, ATP is the most important, energy-rich metabolite in the cell. It's like the equivalent of the dollar for bioenergy clinics in the economy. And ATP, when it appears all of a sudden outside of the cell, is considered as non-physiological. It is a dangerous signal. It is perceived by so-called purinergic receptors that are present, among other cell types, on leukocytes, and particularly myeloid cells. And a cell that undergoes autophagy may, especially, when this occurs before cell death, release ATP to attract myeloid cells into its proximity and to start an immune response against tumor antigens in the context of the initial oncogenic events. And so, autophagy is required for some steps of the immunosurveillance process. And it is exactly this process that makes cancer therapies efficient. So, in contrast to the official dogma that has been en vogue for several decades, chemotherapy is not just killing the cancer cells as if we used an antibiotic that specifically paralyzes the metabolism of bacteria. No. It is true that chemotherapy induces cancer cell death, but the important point is that chemotherapy must provoke this cell death in a way that it later leads to an immune response. And so, if you have a long-term effect of chemotherapy, for years or decades, that continues beyond removal of the drug, it is due to an anti-cancer immune response. And so, since this is so important, the capacity of the chemotherapeutic agent to induce autophagy is actually required for the long-term efficacy of the treatment.
- Rhonda: ... some of your work with the fasting, so-called fasting mimetics like spermidine, hydroxycitrate that you've done. Maybe can you kind of just briefly explain... I'll start with spermidine. What is spermidine? What does it do?
- Dr. Kroemer: Well, it was first start to explain what are these fasting mimetics is as you say and caloric restriction mimetics as we say. So the CRM's, caloric restriction mimetics, are actually inducing the same biochemical changes in the cells as would do starvation or fasting. So, we have been discussing on the importance of acetyl-CoA and protein deacetylation resulting from the inhibition of Acetyl-CoA in the context of fasting. And caloric restriction mimetics, similar induced deacetylation reactions to stimulate autophagy. And this can be actually achieved in three different ways. First, you simply inhibit the generation of Acetyl-CoA. The enzyme that generates Acetyl-CoA in our cells, the most important one for the cytosolic pool, is ATP citrate lyase and hydroxycitrate or pharmacological compounds that inhibit this enzyme cause Acetyl-CoA depletion, deacetylation, and autophagy. And you can have the same effect by inhibiting the protein acetyltransferases, some of them have been identified. Like, EP300 which appears extremely important for autophagy regulation, and specific inhibitors of EP300 such as spermidine and natural compound or C646 which is a pharmacological compound specifically designed for this function. They can also cause deacetylation and autophagy. And finally, it is possible to activate deacetylases or enzymes that remove acetyl groups from proteins and cause hypoacetylation and autophagy. And one example that is well known is resveratrol contained in red wine that induces autophagy through this pathway. So, all these agents, caloric restriction mimetics, have different molecular targets, but activate autophagy by a final common pathway.
- Rhonda: The protein acetylation seems like that.
- Dr. Kroemer: Yes, exactly.
- Rhonda: Okay. So, with some of the major ones that you've worked with, spermidine. I've read quite a bit about spermidine. I know it's found in high concentrations in natto, the Japanese fermented soybean that doesn't taste like great. But I've seen studies about aging, you know, giving it to even aging mice or something, can then extend their lifespan. Is that true?
- Dr. Kroemer: So spermidine, to come to the source of spermidine is contained in the nuclei of all kind of cells. So, in the nucleoid of bacteria but also the nuclei from yeast cells or from plant cells or animal cells. So, all food items that contain nuclei cells, are actually containing spermidine. Also, there are large variations in the content. So we have to know, on this spermidine, it also is volatile and accounts for the smell of sperm. So, it is frequently found in food items that have some kind of smell like natto or durian fruit or fermented cheese, when it is generated from non pasteurized sources and very rich in bacteria and fungi that are contributing to the fermentation process, which is, of course, smelly cheese. And it's also quite abundant in some vegetables and food where the scent is more agreeable to most people because it is complex to other molecules that reduce its volatility. So spermidine has the capacity to induce autophagy when it is taken up with food or with the drinking water when we take mice. It can also be injected, of course. It is produced by our microbiota. So, one-third of the spermidine in our body is probably produced in the intestine, and you can manipulate a microbiome to increase its production of polyamines, including spermidine.
- Rhonda: Through what? Probiotics? Or through...
- Dr. Kroemer: Yes.
- Rhonda: So you know what strains of bacteria... ?
- Dr. Kroemer: Yeah, there is a Japanese group that has been publishing that specific bacteria overproducing polyamines can be used to reduce the development of colon cancer or to reduce aging.
- Rhonda: Wow, fascinating. That's very interesting. And you've shown with the spermidine, I know we have a limited time here, with the spermidine that's been shown to... Was it spermidine or hydroxycitric, I think, that was shown to synergize with, like you were mentioning before, the chemotherapeutic...
- Dr. Kroemer: Yeah, both of them actually.
- Rhonda: Both? Okay.
- Dr. Kroemer: So the mechanism is that when you combine chemotherapy with caloric restriction mimetics, all the caloric restriction mimetics that I mentioned, including spermidine and hydroxycitrate and resveratrol, will enhance the anti-cancer immune response that makes the therapy durable. So, we have been able to show that inhibition of autophagy in the malignant cells or destruction of the extracellular ATP that is released as a result of autophagy is sufficient to abolish the favorable interaction between caloric restriction mimetics and chemotherapy. And similarly, actually, it is sufficient to remove T-cells from the system. And you will lose any kind of tumor growth reduction induced by chemotherapy combined with caloric restriction mimetics as it proves that the cellular immune response is actually decisive for therapeutic outcome.
- Rhonda: Wow, that's really quite promising, I think, for you know at least in the clinic, if you can somehow test whether or not this caloric restriction or fasting mimetics work in conjunction with some of these immunotherapies, that would be fantastic. But I want to ask you one last thing too about some of these fasting mimetics. Like, if I were to just supplement with hydroxycitric, for example, or if there were spermidine supplement, and I was still eating a normal, you know, healthy diet, but not caloric restricted and not fasting. Do you think that would be sufficient to induce autophagy?
- Dr. Kroemer: Well, I can respond for mice...
- Rhonda: Okay. How about in mice?
- Dr. Kroemer: ...that this is certainly the case. I don't know about humans because we have no clinical studies in this field.
- Rhonda: So in mice, it does?
- Dr. Kroemer: It does. And in mice, you actually can give a combination of high-fat diets, that usually would cause obesity, with spermidine to reduce weight gain through mechanisms that we don't understand and that we believe to be autophagy-dependent but have to elucidate in some molecular detail.
- Rhonda: That's very cool. So I'm going to look up those strains of bacteria, you know, to see that can I eat fermented foods to increase that population and get more spermidine. You know, things like that would be very interesting to me as useful little tools. Do you have any practices that you do? Do you, for example, do intermittent fasting or any type of fasting or time-restricted eating?
- Dr. Kroemer: So, usually in my ordinary life, when I'm in Paris and working, I only have one meal per day. So I have dinner with cheese and wine containing spermidine and resveratrol. It's an ideal combination because inhibiting the acetyltransferase and activating the deacetylase will have, of course, a synergistic effect.
- Rhonda: Oh, you do?
- Dr. Kroemer: Well, if you can show this in mice and this is an excuse for me to...
- Rhonda: Yeah, wine and cheese go great together.
- Dr. Kroemer: ...profit from a banquet combination. And I do also practice some fasting twice per year also when I don't eat anything for five days.
- Rhonda: Oh, wow. So you do a prolonged fast twice a year.
- Dr. Kroemer: Well, it's not so prolonged, so you know that Gandhi, for instance, has been doing fasting exercises for 20 days or more, which is the time at which a normal individual could have some long-term consequences on the health. So, 20 days is some period that usually is could be easily supported by a healthy middle-aged individual that has no underlying pathologies.
- Rhonda: I have a couple of friends that have done. One of them is used to very prolonged fast, like 20 days. He's morbidly obese, and he's lost now like 200 pounds over the course of a year by doing just several rounds of these prolonged fasts. But he's got a lot of fat, you know, to supply energy. I'm not sure I would still subject myself to a 20-day water fast, but it's cool to know that you do these five-day water fast, twice a year, and eating one meal a day.
- Dr. Kroemer: Yeah, and doing exercise.
- Rhonda: And doing exercise. And when you're eating... Sorry, throughout the day, when you're not eating, do you drink coffee?
- Dr. Kroemer: Yes.
- Rhonda: And there's polyphenols in coffee that actually...
- Dr. Kroemer: Yes, we published a study in mice giving them a non-toxic dose of caffeinated or decaffeinated coffee with a drinking water continuously. And we could show that this was magnificently inducing autophagy. Like caffeine independent fasting.
- Rhonda: Right, totally independent caffeine, so just the polyphenols. And this was like, I think, I read your study, it was like after four hours or something in the mice. So, in humans, potentially, maybe the fasting plus the coffee...
- Dr. Kroemer: Well, coffee abuse has been linked to major health-promoting effects. So, most cardiovascular and neurodegenerative diseases are actually reduced in heavy coffee drinkers as an independent link between lifestyle and pathology. So, of course, it's an association that obviously can be criticized because it's just a study in which you find a statistical correlation. It would be much more interesting to do a randomized clinical trial on coffee intake.
- Rhonda: More interesting and more expensive, yeah.
- Dr. Kroemer: Yeah. Absolutely.
- Rhonda: Great. So fasting, coffee, wine and cheese, one meal, exercise, you're doing it all. Awesome. Well, really enjoyed this conversation, Guido. If people want to find you, you have a lab website, kroemerlab.com. That's K-R-O-E-M-E-R lab, L-A-B .com. So, thank you again for this wonderful, very illuminating conversation.
- Dr. Kroemer: It's a pleasure.
- Rhonda: I hope you enjoyed learning about all things autophagy, both macro and micro from Dr. Guido Kroemer. Dr. Kroemer in my mind is the consummate expert in this field, and also is amazingly prolific with somewhere in the neighborhood of a thousand publications to his name. Quite the feat to say the least, and all of the more reason why it was an enormous privilege to get to talk to him. Do you love these geeky, deep biology podcasts? You can be a part of the community that nurtures the existence of this podcast and other useful creative offshoots that can be found at FoundMyFitness by heading over to foundmyfitness.com/crowdsponsor. About to buy a solar-powered wood chipper or a gargantuan vat of gee? If you get them from Amazon, make sure to click the FoundMyFitness affiliate link first. Any time you click our Amazon affiliate link, it actually makes sure the podcast will get a small cut for any orders you make in the next 24 hours. It literally doesn't affect your transaction at all. And the best part is you probably already shop at Amazon anyway. No big deal, right? You can find the Amazon affiliate link, as well as other great ways to support the podcast, such as the Pay What You Can subscription, either direct or through Patreon, by heading over to foundmyfitness.com/crowdsponsor That's foundmyfitness.com/ C-R-O-W-D-S-P-O-N-S-O-R Crowd Sponsor. Finally, are you a genetics geek? If you've done your 23andMe, and already have your raw genetic data available to you, you can run it through the genome analysis tool on my website at foundmyfitness.com/genetics. That's foundmyfitness.com/genetics. What's that? You may ask. This tool is a way for me to tell you about interesting single nucleotide polymorphisms, that's SNIPs for short, and to quickly check your raw data for them. Maybe you've heard me talk about a polymorphism that affects how you metabolize saturated fat or vitamin D or any number of other polymorphisms that I've talked about that usually share the common theme of being diet or lifestyle modifiable. Since I'm still learning, my report is still learning, and I'll be adding more and more interesting genetic polymorphisms to the report as time goes on. Definitely worth checking out if you have your 23andMe data or, in the near future, ancestry.com or any of the other genetic providers. We'll be adding those soon. Learn more by heading over to foundmyfitness.com/genetics. Thanks so much for listening and I'll catch you next time.
Acetyl coenzyme A is a molecule that was first discovered to transfer acetyl groups to the citric acid cycle (Krebs cycle) to be oxidized for energy production. Now it is known to be involved in many different pathways including fatty acid metabolism, steroid synthesis, acetylcholine synthesis, acetylation, and melatonin synthesis.
An energy-carrying molecule present in all cells. ATP fuels cellular processes, including biosynthetic reactions, motility, and cell division by transferring one or more of its phosphate groups to another molecule (a process called phosphorylation).
A protein present in the human brain, found primarily at the synapses – the junctions between neighboring neurons where the exchange of electrical signals and neuronal communication occurs. Aggregation, or clumping, of alpha-synuclein proteins is a hallmark of Parkinson's disease, a neurodegenerative disorder of the central nervous system. Hsp70, a heat shock protein, has been shown to reduce formation of alpha-synuclein oligomers and reduce associated toxicity.[1]
- ^ Hashimoto, Tadafumi; J. McLean, Pamela; Danzer, Karin M.; Ruf, Wolfgang P.; Putcha, Preeti; Joyner, Daniel, et al. (2010). Heat‐shock Protein 70 Modulates Toxic Extracellular Α‐Synuclein Oligomers And Rescues Trans‐Synaptic Toxicity The FASEB Journal 25, 1.
A neurodegenerative disorder characterized by progressive memory loss, spatial disorientation, cognitive dysfunction, and behavioral changes. The pathological hallmarks of Alzheimer's disease include amyloid-beta plaques, tau tangles, and reduced brain glucose uptake. Most cases of Alzheimer's disease do not run in families and are described as "sporadic." The primary risk factor for sporadic Alzheimer's disease is aging, with prevalence roughly doubling every five years after age 65. Roughly one-third of people aged 85 and older have Alzheimer's. The major genetic risk factor for Alzheimer's is a variant in the apolipoprotein E (APOE) gene called APOE4.
An enzyme that plays multiple roles in cellular energy homeostasis. AMP kinase activation stimulates hepatic fatty acid oxidation, ketogenesis, skeletal muscle fatty acid oxidation, and glucose uptake; inhibits cholesterol synthesis, lipogenesis, triglyceride synthesis, adipocyte lipolysis, and lipogenesis; and modulates insulin secretion by pancreatic beta-cells.
Programmed cell death. Apoptosis is a type of cellular self-destruct mechanism that rids the body of damaged or aged cells. Unlike necrosis, a process in which cells that die as a result of acute injury swell and burst, spilling their contents over their neighbors and causing a potentially damaging inflammatory response, a cell that undergoes apoptosis dies in a neat and orderly fashion – shrinking and condensing, without damaging its neighbors. The process of apoptosis is often blocked or impaired in cancer cells. (May be pronounced “AY-pop-TOE-sis” OR “AP-oh-TOE-sis”.)
An enzyme that converts citrate into acetyl CoA, which leads to protein acetylation and thus inhibits autophagy. The production of acetyl CoA also represents an important step in fatty acid biosynthesis and by converting citrate to acetyl CoA, ATP citrate lyase links the metabolism of carbohydrates, which yields citrate as an intermediate, to the production of fatty acids, which requires acetyl CoA. Hydroxy citrate is a competitive inhibitor of ATP citrate lyase and thereby reduces the cytosolic levels of acetyl CoA.
↓ ATP citrate lyase activity → ↓ Protein Acetylation → Autophagy
An intracellular degradation system involved in the disassembly and recycling of unnecessary or dysfunctional cellular components. Autophagy participates in cell death, a process known as autophagic dell death. Prolonged fasting is a robust initiator of autophagy and may help protect against cancer and even aging by reducing the burden of abnormal cells.
The relationship between autophagy and cancer is complex, however. Autophagy may prevent the survival of pre-malignant cells, but can also be hijacked as a malignant adaptation by cancer, providing a useful means to scavenge resources needed for further growth.
A protein that regulates autophagy and mediates the vesicle-trafficking processes, which, in eukaryotic cells, involves an organelle known as the Golgi apparatus. Beclin 1 is thought to play a role in multiple cellular processes, including tumorigenesis, neurodegeneration and apoptosis.
The process by which fatty acid molecules are broken down. Beta-oxidation occurs in the mitochondria and produces acetyl-CoA, FADH2, NADH, and H+. Under conditions where glucose is limited, beta-oxidation is an important preceding step for producing the acetyl-CoA needed for ketogenesis.
A measurable substance in an organism that is indicative of some phenomenon such as disease, infection, or environmental exposure.
The practice of long-term restriction of dietary intake, typically characterized by a 20 to 50 percent reduction in energy intake below habitual levels. Caloric restriction has been shown to extend lifespan and delay the onset of age-related chronic diseases in a variety of species, including rats, mice, fish, flies, worms, and yeast.
Compounds that induce a similar biochemical milieu in the cell as starvation or nutrient deprivation, including the reductions in cytosolic acetyl CoA and increases in protein deacetylation that serve as a trigger for the cellular autophagic machinery. Popular examples of compounds that exhibit this type of effect include: hydroxycitrate (inhibits ATP citrate lyase), spermidine (inhibits Ep300, a protein acetyltransferase), and resveratrol (activates deacetylases called sirtuins).
A medication used to prevent and to treat malaria. It is also occasionally used for amebiasis that is occurring outside of the intestines, rheumatoid arthritis, and lupus erythematosus. Currently it is being researched as an antiretroviral in humans with HIV-1/AIDS, an agent in chemotherapy for cancer, and its ability to inhibit lysosomal degradation of protein products during autophagy.
The aqueous component of the cytoplasm of a cell, within which various organelles and particles are suspended.
The biological process in which a cell matures and specializes. Differentiation is essential for the development, growth, reproduction, and lifespan of multicellular organisms. Differentiated cells can only express genes that characterize a certain type of cell, such as a liver cell, for example.
A type of organelle in the cells of eukaryotic organisms that forms as interconnected network of flattened, membrane-enclosed sacs or tube-like structures known as cisternae. Rough ER is studded with ribosomes and is the site of protein synthesis, whereas smooth ER functions in lipid manufacture and metabolism.
Any of a group of complex proteins or conjugated proteins that are produced by living cells and act as catalyst in specific biochemical reactions.
Also known as p300 HAT. A histone acetyltransferase that acetylates proteins in chromatin, causing widespread changes in gene activation. This enzyme can be inhibited by compounds such as spermidine and thereby promote autophagy.
A diet that mimics the effects of fasting on markers associated with the stress resistance induced by prolonged fasting, including low levels of glucose and IGF-1, and high levels of ketone bodies and IGFBP-1. More importantly, evidence suggests these changes in the cellular milieu are associated with a sensitization of cancer cells to chemotherapeutic drugs while simultaneously also conferring greater stress resistance to healthy cells.[1] Evidence also continues to emerge that properties of the fasting-mimicking diet, particularly its ability to cause immune cell turnover, may also make it useful in the amelioration of auto-immune diseases like multiple sclerosis.[2]
Fasting-Mimicking Diet Breakdown
- Day 1 - consists of 1,090 total calories (10% protein, 55% fat and 34% carbohydrate)
- Days 2 through 5 - consists of 725 total calories (9% protein, 44% fat and 47% carbohydrate)
[1] Cheng, Chia-Wei, et al. "Prolonged fasting reduces IGF-1/PKA to promote hematopoietic-stem-cell-based regeneration and reverse immunosuppression." Cell Stem Cell 14.6 (2014): 810-823. [2] Choi, In Young, et al. "A diet mimicking fasting promotes regeneration and reduces autoimmunity and multiple sclerosis symptoms." Cell Reports 15.10 (2016): 2136-2146.
A molecule composed of carboxylic acid with a long hydrocarbon chain that is either saturated or unsaturated. Fatty acids are important components of cell membranes and are key sources of fuel because they yield large quantities of ATP when metabolized. Most cells can use either glucose or fatty acids for this purpose.
A device involved in cell counting, sorting, biomarker detection and protein engineering. Modern versions of a flow cytometer are usually laser-based.
One of the most abundant non-essential amino acids in the human body. Glutamine plays key roles in several metabolic functions, including protein and glutathione synthesis, energy production, antioxidant status, and immune function. In addition, it regulates the expression of several genes. Although the body can typically produce all the glutamine it needs, during periods of metabolic stress it must rely on dietary sources of glutamine such as meats, fish, legumes, fruits, and vegetables.
A series of enzyme-dependent reactions that breaks down glucose. Glycolysis converts glucose into pyruvate, releasing energy and producing ATP and NADH. In humans, glycolysis occurs in the cytosol and does not require oxygen.
A naturally occurring substance capable of stimulating cellular growth, proliferation, healing, and differentiation. Growth factors typically act as signaling molecules between cells. Examples include cytokines and hormones that bind to specific receptors on the surface of their target cells.
A family of proteins produced by cells in response to exposure to stressful conditions. Heat shock proteins are expressed in response to heat as well as exposure to cold and UV light, and during wound healing and tissue remodeling. Many heat shock proteins function as chaperones by stabilizing new proteins to ensure correct folding or by helping to refold proteins that were damaged by cell stress. A 30-minute 73ºC sauna session in healthy young adults has been shown to cause a robust and sustained increase in the production of heat shock proteins for up to 48 hours afterward.[1]
- ^ Shields, Richard K; Iguchi, Masaki; Littmann, Andrew E.; Chang, Shuo-Hsiu; Wester, Lydia A.; Knipper, Jane S. (2012). Heat Stress And Cardiovascular, Hormonal, And Heat Shock Proteins In Humans Journal Of Athletic Training 47, 2.
A critical element of the body’s immune response. Inflammation occurs when the body is exposed to harmful stimuli, such as pathogens, damaged cells, or irritants. It is a protective response that involves immune cells, cell-signaling proteins, and pro-inflammatory factors. Acute inflammation occurs after minor injuries or infections and is characterized by local redness, swelling, or fever. Chronic inflammation occurs on the cellular level in response to toxins or other stressors and is often “invisible.” It plays a key role in the development of many chronic diseases, including cancer, cardiovascular disease, and diabetes.
A peptide hormone secreted by the beta cells of the pancreatic islets cells. Insulin maintains normal blood glucose levels by facilitating the uptake of glucose into cells; regulating carbohydrate, lipid, and protein metabolism; and promoting cell division and growth. Insulin resistance, a characteristic of type 2 diabetes, is a condition in which normal insulin levels do not produce a biological response, which can lead to high blood glucose levels.
One of the most potent natural activators of the AKT signaling pathway. IGF-1 stimulates cell growth and proliferation, inhibits programmed cell death, mediates the effects of growth hormone, and may contribute to aging and enhancing the growth of cancer after it has been initiated. Similar in molecular structure to insulin, IGF-1 plays a role in growth during childhood and continues later in life to have anabolic, as well as neurotrophic effects. Protein intake increases IGF-1 levels in humans, independent of total caloric consumption.
A broad term that describes periods of voluntary abstention from food and (non-water) drinks, lasting several hours to days. Depending on the length of the fasting period and a variety of other factors, intermittent fasting may promote certain beneficial metabolic processes, such as the increased production of ketones due to the use of stored fat as an energy source. The phrase “intermittent fasting” may refer to any of the following:
- Time-restricted eating
- Alternate-day fasting
- Periodic fasting (multi-day)
Molecules (often simply called “ketones”) produced by the liver during the breakdown of fatty acids. Ketone production occurs during periods of low food intake (fasting), carbohydrate restrictive diets, starvation, or prolonged intense exercise. There are three types of ketone bodies: acetoacetate, beta-hydroxybutyrate, and acetone. Ketone bodies are readily used as energy by a diverse array of cell types, including neurons.
A type of white blood cell. Leukocytes are involved in protecting the body against foreign substances, microbes, and infectious diseases. They are produced or stored in various locations throughout the body, including the thymus, spleen, lymph nodes, and bone marrow, and comprise approximately 1 percent of the total blood volume in a healthy adult. Leukocytes are distinguished from other blood cells by the fact that they retain their nuclei. A cycle of prolonged fasting has been shown in animal research to reduce the number of white blood cells by nearly one-third, a phenomenon that is then fully reversed after refeeding.[1]
- ^ Cheng CW; Adams GB; Perin L; Wei M; Zhou X; Lam BS, et al. (2014). Prolonged fasting reduces IGF-1/PKA to promote hematopoietic-stem-cell-based regeneration and reverse immunosuppression. Cell Stem Cell 14, 6.
Macroautophagy is used primarily to eradicate damaged cell organelles or unused and/or damaged proteins. This involves the formation of a double membrane known as an autophagosome around the organelle marked for destruction before delivering it to a lysosome. Microautophagy, on the other hand, involves direct engulfment of cytoplasmic material by the lysosome via a process of invagination, meaning the inward folding of the lysosomal membrane.
A type of white blood cell. Macrophages engulf and digest cellular debris, foreign substances, microbes, cancer cells, and oxidized LDL in a process called phagocytosis. After phagocytizing oxidized LDL, macrophages are referred to as foam cells.
An enzyme that participates in genetic pathways that sense amino acid concentrations and regulate cell growth, cell proliferation, cell motility, cell survival, protein synthesis, autophagy, and transcription. mTOR integrates other pathways including insulin, growth factors (such as IGF-1), and amino acids. It plays key roles in mammalian metabolism and physiology, with important roles in the function of tissues including liver, muscle, white and brown adipose tissue, and the brain. It is dysregulated in many human diseases, such as diabetes, obesity, depression, and certain cancers. mTOR has two subunits, mTORC1 and mTORC2. Also referred to as “mammalian” target of rapamycin.
Rapamycin, the drug for which this pathway is named (and the anti-aging properties of which are the subject of many studies), was discovered in the 1970s and is used as an immunosuppressant in organ donor recipients.
The thousands of biochemical processes that run all of the various cellular processes that produce energy. Since energy generation is so fundamental to all other processes, in some cases the word metabolism may refer more broadly to the sum of all chemical reactions in the cell.
The collection of genomes of the microorganisms in a given niche. The human microbiome plays key roles in development, immunity, and nutrition. Microbiome dysfunction is associated with the pathology of several conditions, including obesity, depression, and autoimmune disorders such as type 1 diabetes, rheumatoid arthritis, muscular dystrophy, multiple sclerosis, and fibromyalgia.
A collective term for the community of commensal, symbiotic, and pathogenic microorganisms that live in a particular environment. The human body has multiple microbiotas, including those of the gut, skin, and urogenital regions.
Tiny organelles inside cells that produce energy in the presence of oxygen. Mitochondria are referred to as the "powerhouses of the cell" because of their role in the production of ATP (adenosine triphosphate). Mitochondria are continuously undergoing a process of self-renewal known as mitophagy in order to repair damage that occurs during their energy-generating activities.
The process by which new mitochondria are made inside cells. Many factors can activate mitochondrial biogenesis including exercise, cold shock, heat shock, fasting, and ketones. Mitochondrial biogenesis is regulated by the transcription factor peroxisome proliferator-activated receptor gamma coactivator 1-alpha, or PGC-1α.
The selective degradation of mitochondria by autophagy. It often occurs in defective mitochondria following damage or stress. Mitophagy is key in keeping the cell healthy. It promotes turnover of mitochondria and prevents accumulation of dysfunctional mitochondria, which can lead to cellular degeneration.
One of four nitrogen-containing molecules that comprise DNA. A nucleotide consists of one of four chemicals, called a “base,” plus one molecule of sugar and one molecule of phosphoric acid. Nucleotides are typically identified by the first letter of their base names: adenine (A), cytosine (C), guanine (G), and thymine (T). They form specific pairs (A with T, and G with C), and their bonds provide the helical structure of the DNA strand.
An oncogene is a mutated form of a gene ordinarily involved in the otherwise healthy regulation of normal cell growth and differentiation. Activation of an oncogene, through mutation of a proto-oncogene, promotes tumor growth. Mutations in genes that become oncogenes can be inherited or caused by environmental exposure to carcinogens. Some of the most common genes mutated in cancer are the IGF-1 receptor and its two main downstream signaling proteins: Ras and Akt.
A gene that has the potential to cause cancer. A proto-oncogene is a normal gene that regulates cell growth and proliferation but if it acquires a mutation that keeps it active all the time it can become an oncogene that allows cancer cells to survive when they otherwise would have died.
A chemical reaction in which an atom, molecule, or ion loses one or more electrons. Oxidation of biological molecules is associated with oxidative stress, a key driver of many chronic diseases.
The process of generating energy that occurs when mitochondria couple oxygen with electrons that have been derived from different food sources including glucose, fatty acids, and amino acids.
A neurodegenerative disorder that affects the central nervous system. Parkinson’s disease is caused by destruction of nerve cells in the part of the brain called the substantia nigra. It typically manifests later in life and is characterized by tremors and a shuffling gait.
Shared characteristics between different organisms due to similar ancestry
A biological pathway involved in mitochondrial function and surveillance. Severely damaged mitochondria lack sufficient membrane potential to import PINK1, which then accumulates on the outer membrane. PINK1 then recruits parkin to target the damaged mitochondria for degradation through autophagy. Due to the presence of PINK1 throughout the cytoplasm, PINK1 likely functions as a "scout" to probe for damaged mitochondria. Point or truncation mutations in PINK1 that reduce the kinase activity of the protein produce Parkinson’s disease with a broad phenotypic spectrum, from early-onset with atypical features to typical late-onset Parkinson’s disease.[1]
- ^ Blomgren, Klas; Kroemer, Guido (2007). Mitochondrial Cell Death Control In Familial Parkinson Disease PLOS Biology 5, 7.
A class of chemical compounds produced in plants in response to stressors. Polyphenols contribute to the bitterness, astringency, color, flavor, and fragrance of many fruits and vegetables. They often serve as deterrents to insect or herbivore consumption. When consumed in the human diet, polyphenols exert many health benefits and may offer protection against development of cancers, cardiovascular diseases, diabetes, osteoporosis, and neurodegenerative diseases. Dietary sources of polyphenols include grapes, apples, pears, cherries, and berries, which provide as much as 200 to 300 mg polyphenols per 100 grams fresh weight.
A type of intermittent fasting that exceeds 48 hours. During prolonged periods of fasting, liver glycogen stores are fully depleted. To fuel the brain, the body relies on gluconeogenesis – a metabolic process that produces glucose from ketones, glycerol, and amino acids – to generate approximately 80 grams per day of glucose [1]. Depending on body weight and composition, humans can survive 30 or more days without any food. Prolonged fasting is commonly used in the clinical setting.
[1] Longo, Valter D., and Mark P. Mattson. "Fasting: molecular mechanisms and clinical applications." Cell metabolism 19.2 (2014): 181-192.
A chemical reaction that removes an acetyl functional group from a chemical compound. The presence of the acetyl functional group plays an important role in the synthesis, stability and localization of about 85% of human proteins.[1] During fasting, falling acetyl CoA levels in the cytosol initiate protein deacetylation and initiates autophagy. In general, protein deacetylation, whether from so-called caloric restriction mimetics or nutrient deprivation, is an important general inducer of autophagy.
- ^ Arnesen, Thomas; Van Damme, Petra; Martinho, Rui Gonçalo; Helsens, Kenny; Hole, Kristine; Pimenta-Marques, Ana, et al. (2011). NatF Contributes To An Evolutionary Shift In Protein N-Terminal Acetylation And Is Important For Normal Chromosome Segregation PLOS Genetics 7, 7.
The purinergic receptors, also known as purinoceptors, are divided into two major families: the P1, or adenosine, receptors and P2 receptors, which bind ATP and/or UTP. In the 1970s, adenosine was found to stimulate cAMP formation in brain slices. Subsequently, physiological effects of adenosine on almost all tissues have been described. These receptors have been implicated in learning and memory, locomotor and feeding behavior, and sleep. More specifically, they are involved in several cellular functions, including proliferation and migration of neural stem cells, vascular reactivity, apoptosis and cytokine secretion.
A compound initially developed as an antifungal agent. This use was abandoned, however, when it was discovered to have potent immunosuppressive and antiproliferative properties due to its ability to inhibit one of the complexes of mTOR (mTORC1). Rapamycin has since shown interesting lifespan extension properties in animals.
Oxygen-containing chemically-reactive molecules generated by oxidative phosphorylation and immune activation. ROS can damage cellular components, including lipids, proteins, mitochondria, and DNA. Examples of ROS include: peroxides, superoxide, hydroxyl radical, and singlet oxygen.
A related byproduct, reactive nitrogen species, is also produced naturally by the immune system. Examples of RNS include nitric oxide, peroxynitrite, and nitrogen dioxide.
The two species are often collectively referred to as ROS/RNS. Preventing and efficiently repairing damage from ROS (oxidative stress) and RNS (nitrosative stress) are among the key challenges our cells face in their fight against diseases of aging, including cancer.
A polyphenolic compound produced in plants in response to injury or pathogenic attack from bacteria or fungi. Resveratrol exerts a diverse array of biological effects, including antitumor, antioxidant, antiviral, and hormonal activities. It activates sirtuin 1 (SIRT1), an enzyme that deacetylates proteins and contributes to cellular regulation (including autophagy). Dietary sources of resveratrol include grapes, blueberries, raspberries, and mulberries.
Resveratrol Autophagy ↑ Deacetylases (especially SIRT1) → ↓ Protein Acetylation → Autophagy
A long-term autoimmune disorder that primarily affects joints. It typically results in warm, swollen, and painful joints. Pain and stiffness often worsen following rest. Most commonly, the wrist and hands are involved. The underlying mechanism involves the body's immune system attacking the joints.
A polyamine (an organic compound having more than two amino groups) named for having been isolated in semen. Spermidine has since been found in a variety of different tissue types, as well as foods. It is best known for its role as a potential autophagy and longevity promoter with its effects having been demonstrated in yeast, flies, worms, and human immune cells.[1]
↓ Acetyltransferase activity (especially EP300) → ↓ cytosolic Acetyl CoA → Autophagy
↓ mitochondrial transmembrane potential → ↑ ubiquitination → mitophagy (preferentially targeted)
- ^ Hartl, Regina; Megalou, Evgenia; Laun, Peter; Heeren, Gino; Breitenbach, Michael; Grubeck-Loebenstein, Beatrix, et al. (2009). Induction Of Autophagy By Spermidine Promotes Longevity Nature 11, 11.
Genes that suppress cell division or growth. Tumor suppressor genes encode proteins involved in aspects of cell growth regulation such as cell cycle arrest and apoptosis. Loss of tumor suppressor gene function promotes uncontrolled cell division and growth, which are hallmarks of cancer.
Ubiquitin is a small regulatory protein found in most tissues of eukaryotic organisms (e.g. ubiquitously). Ubiquitination refers to the the process by which ubiquitin proteins are added to cytosolic proteins in order to: alter their cellular location, mark them for degradation via the proteasome, and promote or prevent protein interactions.
Formed into or containing one or more vacuoles or small membrane-bound cavities within a cell.
A fat-soluble vitamin stored in the liver and fatty tissues. Vitamin D plays key roles in several physiological processes, such as the regulation of blood pressure, calcium homeostasis, immune function, and the regulation of cell growth. In the skin, vitamin D decreases proliferation and enhances differentiation. Vitamin D synthesis begins when 7-dehydrocholesterol, which is found primarily in the skin’s epidermal layer, reacts to ultraviolet light and converts to vitamin D. Subsequent processes convert D to calcitriol, the active form of the vitamin. Vitamin D can be obtained from dietary sources, too, such as salmon, mushrooms, and many fortified foods.
Member only extras:
Learn more about the advantages of a premium membership by clicking below.
Supporting our work
If you enjoy the fruits of
 , you can participate in helping us to keep improving it. Creating a premium subscription does just that! Plus, we throw in occasional member perks and, more importantly, churn out the best possible content without concerning ourselves with the wishes of any dark overlords.
, you can participate in helping us to keep improving it. Creating a premium subscription does just that! Plus, we throw in occasional member perks and, more importantly, churn out the best possible content without concerning ourselves with the wishes of any dark overlords.